Optimising the arterial phase
Key Learnings:
- Background of artifacts that can potentially impact the arterial phase of a Gadoxetate disodium(Gd-EOB-DTPA) Liver MRI
- Theory of bolus geometry, relaxivity and timing the arterial phase in the liver with Gadoxetate disodium(Gd-EOB-DTPA)
- Techniques to mitigate the appearance of artifacts in the arterial phase with Gadoxetate disodium(Gd-EOB-DTPA).
Kristie Smith is a qualified radiographer in Australia, topping her graduating class from University of Sydney in 2006. She has medical imaging experience in general x-ray, mammography, CT, fluoroscopy and over 10 years’ clinical experience in MRI; the last 6 years working as a Senior MR radiographer.
About this webinar:
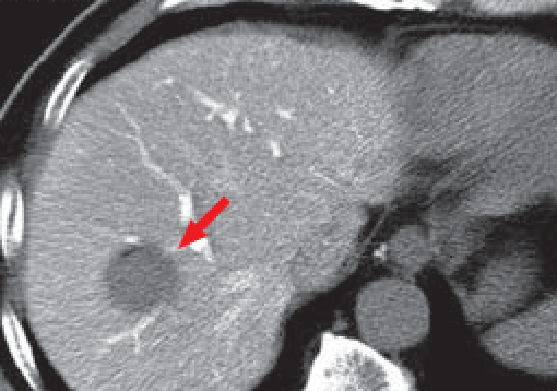
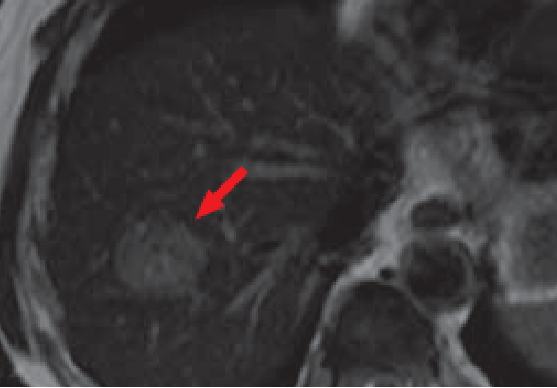
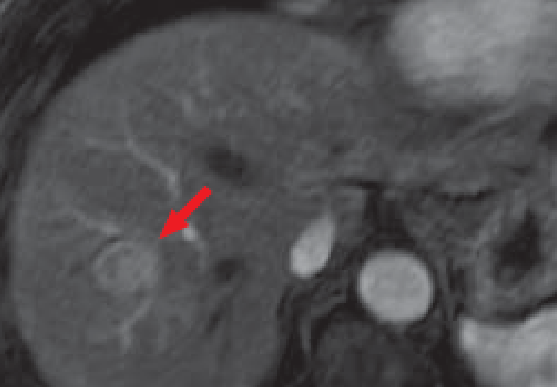
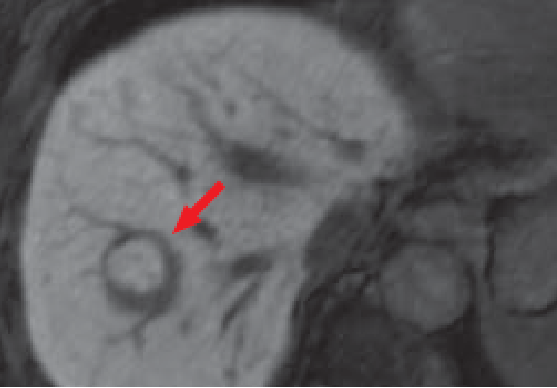
The arterial phase in a liver MRI with Gadoxetate disodium(Gd-EOB-DTPA) is important in identifying and classifying focal liver lesions based on their enhancement patterns. Transient respiratory motion and truncation artifact can potentially impact the image quality of the arterial phase. These artifacts can be potentially lessened through utilizing a number of strategies, including optimized Gadoxetate disodium(Gd-EOB-DTPA) injection, appropriate timing of the arterial phase and patient instructions, and using mutli-arterial sequences.
Introduction and artifacts in liver imaging (10 minutes)
- Hepatobiliary phase
- Arterial phase & potential challenge (artifacts and timing)
- Transient respiratory motion (TRM): definition, prevalence
- Truncation artifact
- Risk factor of TRM: Previous TRM, COPD, age, BMI, breath hold capacity
Proposed strategies for arterial phase optimization: injection rate and acquisition timing (12.5 minutes)
- Injection rate: slower injection rate for bolus, relaxivity, and protein binding
- Power injection
- Saline flush
- Fluoroscopic triggering
Proposed strategies for arterial phase optimization : Patient Preparation (10 minutes)
- breath hold command
- Sequence strategies: multi-arterial phases
- Oxygen inhalation
- Summary