The targetoid appearance of EOB-MRI in differentiating mass-forming intrahepatic cholangiocarcinoma from hepatocellular carcinoma.
Taipei Veterans General Hospital
Chien-An Liu, Division of Abdominal Imaging, Department of Radiology, Taipei Veterans General Hospital, Taipei, Taiwan.
Yi-Ping Hung, Department of Oncology, Taipei Veterans General Hospital, Taipei, Taiwan.
DATE : 2024
Introduction

Patient’s background
62 years old, Male, 60.4kg
Disease(s): Cholangiocarcinoma (CCA)
Patient characteristics and purpose of contrast-enhanced MRI
This 62-year-old gentleman without underlying disease was incidentally found to have a 12.7cm hepatic tumor by triple-phase CT scan in a health check-up. The CT findings suggest the diagnosis of atypical hepatocellular carcinoma (HCC) or Combined hepatocellular-cholangiocarcinoma (cHCC-CCA)(Fig.1). Then he was admitted to our hospital for a second opinion. Tumor markers such as alpha-fetoprotein (AFP), carbohydrate antigen 19-9 (CA19-9), and carcinoma embryonic antigen (CEA) levels were within normal limits. The Gd-EOB-DTPA enhanced MRI was arranged for further evaluation.
Contrast agent used
Gadoxetate disodium(Gd-EOB-DTPA) injection, 0.1 mL/kg
Case description
In EOB-MRI images(Fig.2), the tumor shows peripheral arterial enhancement, progressive central enhancement in portovenous, and target-like appearance of the wash-out in the late-venous phase. Targetoid appearance on 20 mins hepatobiliary phase (HBP) was noted as well. According to CT/MRI LI-RADs criteria and lacking a typical vascular pattern for HCC, the main tumor was defined as LR-M. Sonography-guided liver biopsy was done for a conclusive diagnosis. However, an acute bleeding event was found after liver biopsy. The vital signs were stabilized after fluid challenge and blood transfusion. The pathology result was confirmed as cholangiocarcinoma (CCA). Then chemotherapy was arranged with nivolumab, gemcitabine and TS-1. Transarterial radioembolization (TARE) with yttrium 90 resin microsphere (SIR-Spheres; Sirtex Medical Limited, Sydney, Australia) was also performed for further disease control.
Imaging

The initial CT scan showed a 12.7cm mass at the left lobe liver(A,B, C)(asterisk ) with a satellite nodule(arrowhead). The primary tumor revealed hepatic capsular retraction(arrow), hypervascularity with peripheral enhancement in the arterial phase(B), and delayed central enhancement in the portal venous phase(C).
Fig. 1. Triphasic dynamic contrast-enhanced CT scan

EOB-MRI before treatment showed no fat content of the tumor based on in- and out-of-phase images(A, B). T2-weighted image demonstrated moderate T2 hyperintensity with targetoid appearance(C). The arterial phase image revealed target-like enhancement(D), and the delayed-phase image showed progressive enhancement(E), “target-sign” appearance of the wash-out(F) and bright signal on DWI (H). Targetoid appearance can also be seen on 20 min HBP(G) and ADC(I) images.
Fig. 2. Gd-EOB-DTPA enhanced MRI
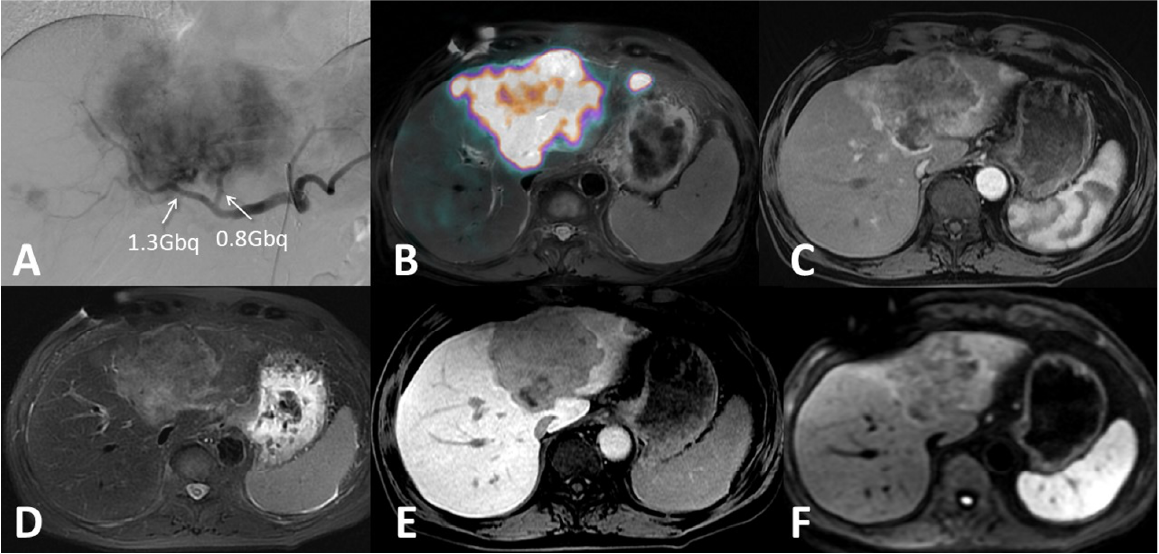
Regarding the TARE(A), 1.3 Gbq and 0.8 Gbq dosing were infused into the tumor-feeding arteries from the right hepatic artery and left hepatic artery separately to provide a tumoricidal dose of more than 120 Gy. The immediate PET/MRI imaging revealed adequate tumor coverage(B). The follow-up EOB-MRI in 3 months showed decreased tumor size and good response imaging patterns1 with the presentations of thin rim peritumoral enhancement(C), reduced T2 signal intensity(D), no newly developed lesion on 20 min HBP(E), and a decrease in DWI signal intensity(F).
Fig. 3. Y90 radioembolization (TARE) and follow-up Gd-EOB-DTPA enhanced MRI
Usefulness of contrast-enhanced MRI with Gadoxetate disodium(Gd-EOB-DTPA) in this case
To differentiate intrahepatic cholangiocarcinoma (ICC) from hepatocellular carcinoma (HCC) is crucial for treatment strategy. The imaging criteria for an observation to be included in the category LR-M (probably or definite malignancy, but not specific for HCC) have been redefined in the LI-RADS v20172. In LI-RADS v20183, targetoid dynamic enhancement includes rim arterial phase hyperenhancement (APHE), peripheral wash-out, delayed central enhancement (DCE), targetoid restriction, targetoid transitional phase(TP), or HBP appearance3.
Targetoid appearance on HBP and targetoid restriction on DWI have been considered independent predictors for differentiating mass-forming ICCs from atypical HCCs (all p=0.001)4. Other factors favoring ICCs include normal AFP, elevated CA19-9 level, high CEA level, central hyperintensity on T2-weighted imaging (T2WI), and central hypointensity on T2WI4. Furthermore, a multicenter retrospective study5 revealed radiologic and clinical factors that may be associated with recurrence and survival after curative surgery for targetoid primary liver malignancies. The poor predictors include tumor size of ≥ 2 cm, thin-rim APHE, HBP hypointense nodules without APHE, and tumor vascular involvement.
In conclusion, the contrast enhancement patterns and targetoid HBP/DWI on EOB-MRI provide a more accurate diagnosis when compared with dynamic CT in this case. Although the patient still received sono-guided biopsy under the condition of clinical trial consideration, some unnecessary biopsy may be waived if the diagnosis can be confirmed by relatively non-invasive evaluation.
Imaging protocol
Devices used and contrast conditions
| MR device used | Signa HDxt 1.5T(GE Healthcare) |
| Autoinjector | LF |
| Workstation | ADW4.5 |
| Contrast enhancement condition | Dose(mL) | Infusion rate (mL/sec) | Imaging timing | |
| Gadoxetate disodium(Gd-EOB-DTPA) | 0.1mL/kg | 1mL/sec | ー | |
| Physiological saline chaser | 30ml | 1mL/sec |
| Imaging type | Imaging sequence | Imaging duration | TE (msec) | TR (msec) | FA (deg) | Fat Sat (Type) | NEX (Number of additions) | k-space | Slice thickness (mm) | FOV (mm) | Phase direction (Number of steps) | Lead direction (Number of matrices) | Slice gap (mm) | Number of slices |
| Dual echo | FSPGR (in & out of phase) | 20" | 2.2 | 178 | 80 | n | 1 | linear | 8 | 32 | 224 | 256 | 2 | 20 |
| With a contrast agent | ||||||||||||||
| Dynamic | LAVA (axial) | 20" | 3.1 (minu- mum) | 6.7 | 12 | y | 1 | linear | 3 | 32 | 192 | 288 | 0 | 100 |
| DWI | EPI (b=800sec/mm2) | 4'44" | 57.1 | 10000 | n | y | 4 | linear | 8 | 32 | 128 | 96 | 2 | 20 |
| T2WI | PROPELLER (axial) | 3' | 97 | 6000 | n | y | 1 | linear | 6 | 32 | 256 | 256 | 0 | 34 |
| HBP (20min) | LAVA (axial) | 20" | 3.1 (minimum) | 6.8 | 12 | y | 1 | linear | 3 | 32 | 192 | 288 | 0 | 100 |
References
MillerFH, VendramiCL, GabrA, HorowitzJM, KelahanLC, RiazA, et al. Evolution of radioembolization in treatment of hepatocellular carcinoma: A pictorial review. Radiographics. 2021;41(6):1802-18.
SchimaW, HeikenJ. LI-RADS v2017 for liver nodules: How we read and report. Cancer Imaging. 2018;18(1):1-11.
RadiologyAC of. CT/MRI LI-RADS v2018. 2018;1-60. Available from:
https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS/CT-MRI-LI-RADS-v2018
HanD, LIY, HeX, ZhangJ, ZhouY, ZhangJ, et al. Differentiating mass-forming intrahepatic cholangiocarcinoma from atypical hepatocellular carcinoma using Gd-EOB-DTPAenhanced magnetic resonance imaging combined with serum markers in at-risk patients with hepatitis B virus. Quant Imaging Med Surg. 2023;13(10):7156-69.
ParkSH, HeoS, KimB, LeeJ, ChoiHJ, SungPS, et al. Targetoid Primary Liver Malignancy in Chronic Liver Disease: Prediction of Postoperative Survival Using Preoperative MRI Findings and Clinical Factors. Korean J Radiol. 2023;24(3):190-203.
- * The case introduced is just one clinical case, so the results are not the same as for all cases.
- * Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


