Evaluation of distant metastasis by contrast computed tomography (CT) after right breast cancer treatment
Gifu University
Dept. of Radiology, Division of Biomedical Medicine, Graduate School of Medicine
Drs. Masayuki Matsuo, Hiroki Kato, Yo Kaneko, Yoshifumi Noda, Nobuyuki Kawai
Dept. of Radiology, Gifu University Hospital
Drs. Yasuhiro Inoue, Toshiharu Miyoshi
DATE : 2021
Introduction

Patient’s background
Female; 40s; body weight: 57 kg; metastatic liver cancer and abdominal lymph node metastasis
Assessment objectives
After preoperative chemotherapy for right breast cancer 6 years previously, partial mastectomy and axillary lymph node dissection had been performed, followed by postoperative radiotherapy and chemotherapy. Metastasis had recurred in the remaining right breast 4 years previously, so mastectomy of the remaining breast had been performed, followed by postoperative chemotherapy. On the present occasion, pulmonary and hepatic masses were found in a health check-up, so it was decided that thorough tests should be performed.
Contrast agent used
Iopromide 370 injection syringe, 88 mL
Case explanation
Distant metastasis is an important prognostic factor for patients with cancer. Accurate recognition of distant metastases is an essential condition for diagnosis of disease stage, and subsequent selection of appropriate treatment. Contrast CT is useful for detection of distant metastases, and is one of the most commonly used modalities. The patient had distant recurrent metastasis after right breast cancer treatment. Whole-body contrast CT was performed, and pulmonary metastasis, hepatic metastasis, and abdominal lymph node metastasis were found, but the images shown are mainly of abdominal lesions.
Imaging findings

Small and large ischemic nodules (arrowheads) were clearly delineated in both hepatic lobes, indicating multiple hepatic metastasis.
A mass (arrow) was found to project to the liver surface in the lateral segment of the left lobe, and it showed marginal, nodular, dark staining, so was considered to be a hemangioma.
Fig. 1. Axial section (umbilical level on portal vein)

Multiple ischemic nodules (arrowheads) were clearly delineated in the lateral segment of the left hepatic lobe, indicating multiple hepatic metastasis.
A mass (arrow) showing marginal, nodular, dark staining was found in the lateral segment of the left lobe, and was considered to be a hemangioma.
Fig. 2. Coronal section reconstruction (left branch level on portal vein)

Multiple ischemic nodules (arrowheads) were clearly delineated at the liver surface, indicating multiple hepatic metastasis.
A mass (arrow) showing marginal, nodular, dark staining was found in the lateral segment of the left hepatic lobe, and was considered to be a hemangioma.
A superior pancreatic head posterior lymph node (※ sign) was swollen, and the interior showed heterogeneous low absorption, showing it to be lymph node metastasis with associated necrosis.
Fig. 3. Coronal section reconstruction (branch level on portal vein)
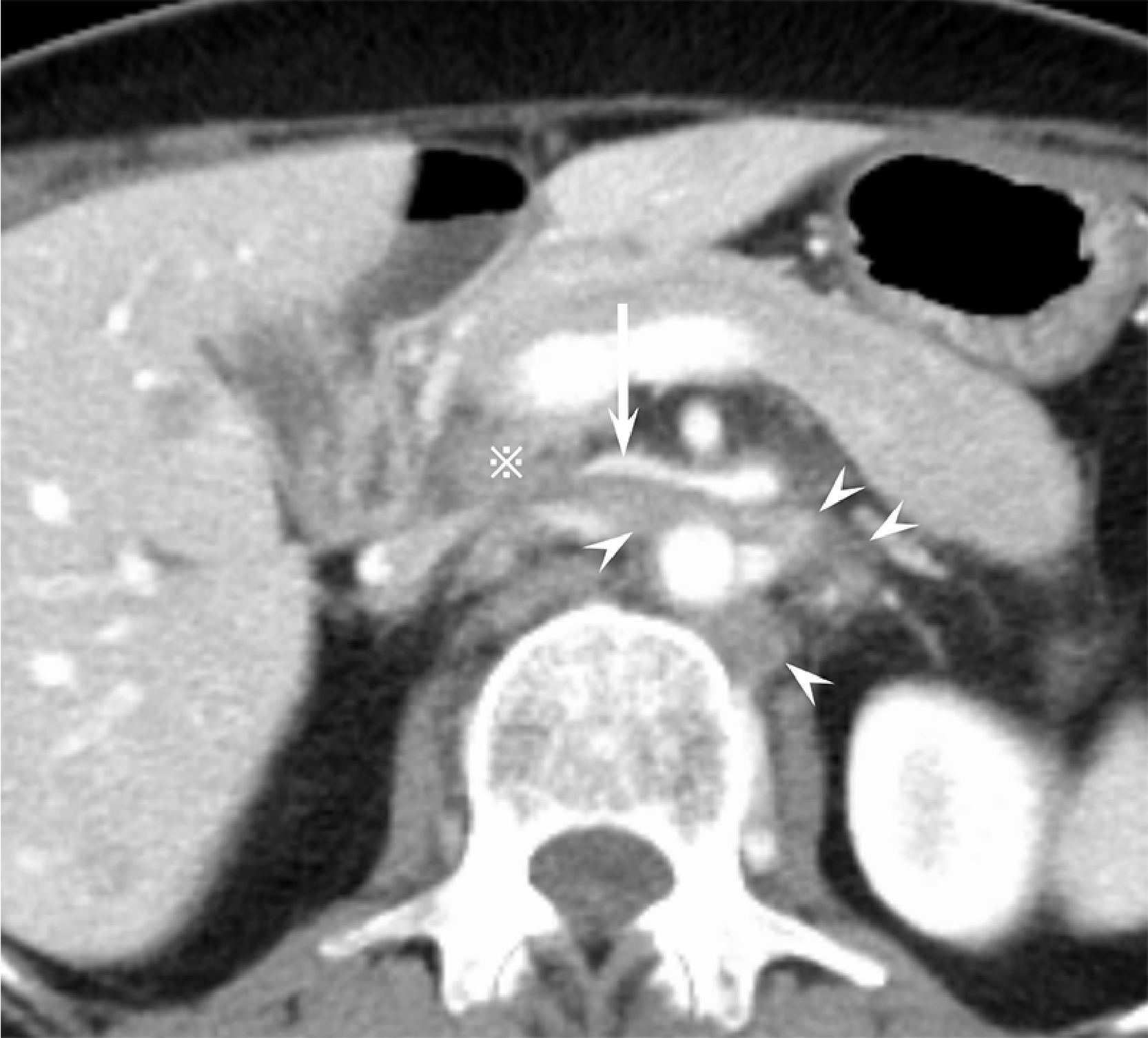
The superior pancreatic head posterior lymph node (※ sign) and paraaortic lymph nodes (arrowheads) were swollen, and the interiors showed heterogeneous low absorption, showing them to be lymph node metastases with associated necrosis.
The left renal vein (arrow) was occluded by the superior pancreatic head posterior lymph node metastasis.
Fig. 4. Axial section (splenic vein level)


Due to the left renal vein occlusion, collateral circulation (arrowhead) had clearly developed from the left ovarian vein to the opposite side.
Figs. 5, 6. Coronal reconstruction images
Photography protocol
| Equipment used | CT device model | Discovery CT750 HD (GE Healthcare Japan) |
| Number of CT detector rows | 64 | |
| Workstation | Advantage Workstation 4.7 (GE Healthcare Japan) |
| Imaging conditions | Imaging phase | Portal phase |
| Tube voltage (kV) | 120 | |
| AEC | 3D mA modulation function used | |
| Noise Index (HU) | 12 | |
| 3D mA modulation function used | ||
| Beamwidth (mm) | 40 | |
| Slice thickness (mm) | 0.625 | |
| Focal-spot size | L | |
| Scan mode | Helical | |
| Scan speed (s/rotation) | 0.5 | |
| Pitch | 0.984:1 | |
| Scan range | Below mandible to pelvic floor | |
| Imaging duration (s) | 9.4 | |
| Imaging direction | Head-to-tail direction |
| Reconstruction conditions | Portal phase | |
| Routine: Reconstructed slice thickness / interval (mm/mm) | 5/5 | |
| Routine: Reconstruction function / iterative approximation method | STND/ASiR-V 40% |
| Contrast conditions | Portal phase | |
| Automatic injector model and manufacturer | Dual Shot GX7 (Nemoto Kyorindo) | |
| Contrast agent used | Iopromide 370 injection syringe | |
| Contrast agent: Dose (mL) | 88 | |
| Contrast agent: Injection duration (s) | 30 | |
| Physiological saline solution: Dose (mL) | ー | |
| Physiological saline solution: Injection speed (mL/s) or injection duration (s) | ー | |
| Scan timing | Fixed delay | |
| Delay time (s) | 65 | |
| Indwelling needle size (G) | 20 | |
| Injection pressure limit (kg/cm2) | 10 |
- *The case introduced is just one clinical case, so the results are not the same as for all cases.
- *Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


