A case of EOB-MRI being useful for assessing therapeutic efficacy against colorectal cancer hepatic metastases
Iwate Medical University Hospital
Dr. Akio Tamura, Dept. of Radiology
Dr. Shun Abe, Division of Central Radiology
DATE : 2021
Introduction

Patient’s background
Male; 40s; colorectal cancer hepatic metastases
Assessment objectives
With this patient, chemotherapy was performed after left hemicolectomy for descending colon cancer with multiple hepatic metastases. After four cycles of Cmab + mFOLFOX6 chemotherapy the control was insufficient, so eight cycles of Pmab + FOLFIRI chemotherapy were performed. Contrast computed tomography (CT) showed almost complete response (CR), but EOB-MRI was performed in order to make a reliable assessment of therapeutic efficacy.
Contrast agent used
Gadoxetate disodium(Gd-EOB-DTPA) injection, 0.1 mL/kg
Case explanation
EOB-MRI showed a residual lesion, so additional treatment was provided. Repeated EOB-MRI after one cycle of Bmab + FOLFILI chemotherapy showed the lesions to have disappeared. Hepatectomy was then performed with the aim of being radical treatment.
Imaging findings
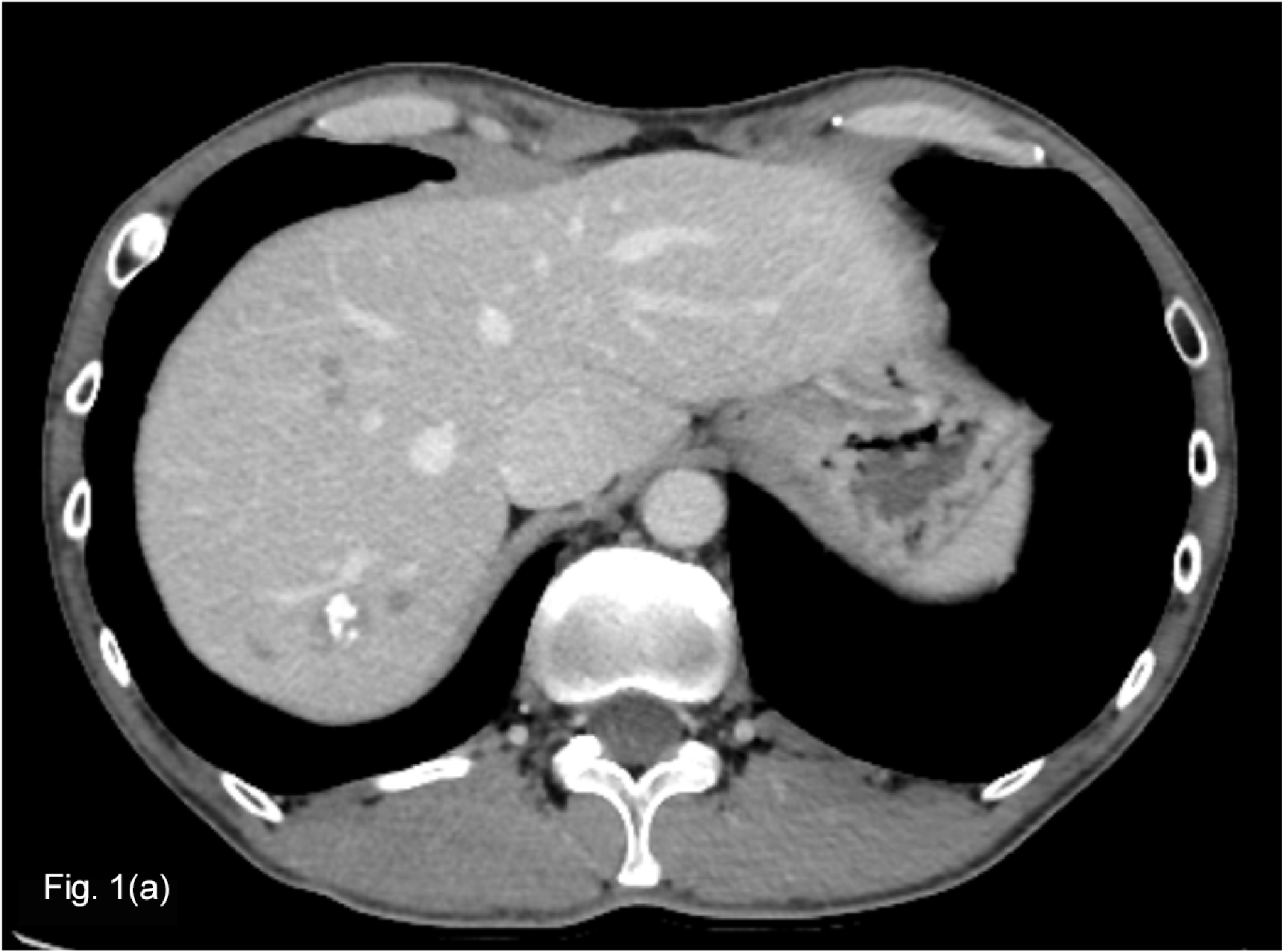

Pretreatment contrast CT (a) showed small lesions suspected of being hepatic metastases in S7 and S8 of the liver.
Cmab + mFOLFOX6 chemotherapy was then initiated, followed by eight cycles of Pmab + FOLFIRI chemotherapy, after which contrast CT (b) suggested minor residual lesions surrounding the calcified lesion in S7, but other hepatic metastases were difficult to identify.
Fig. 1. Contrast CT equilibrium phase
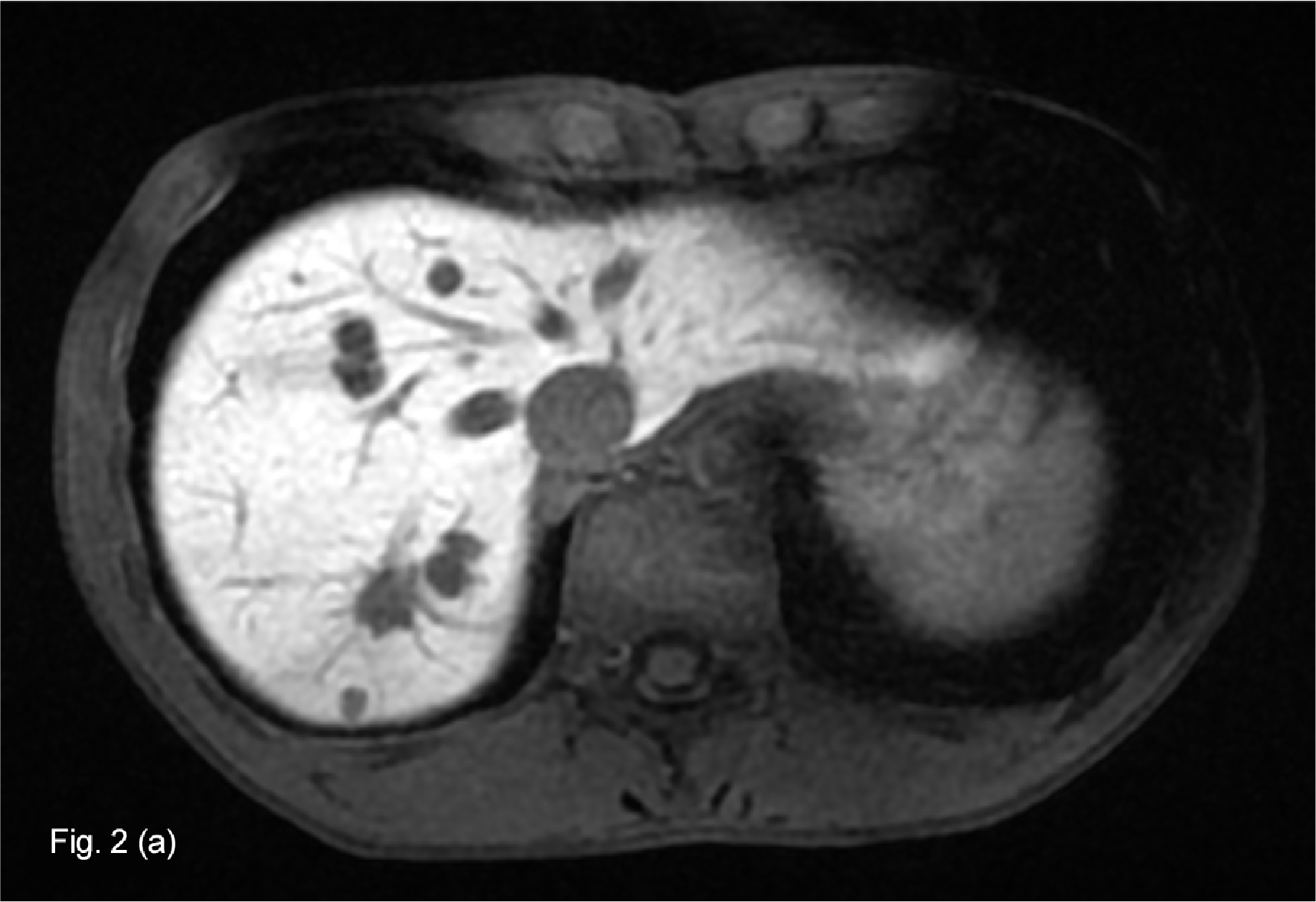
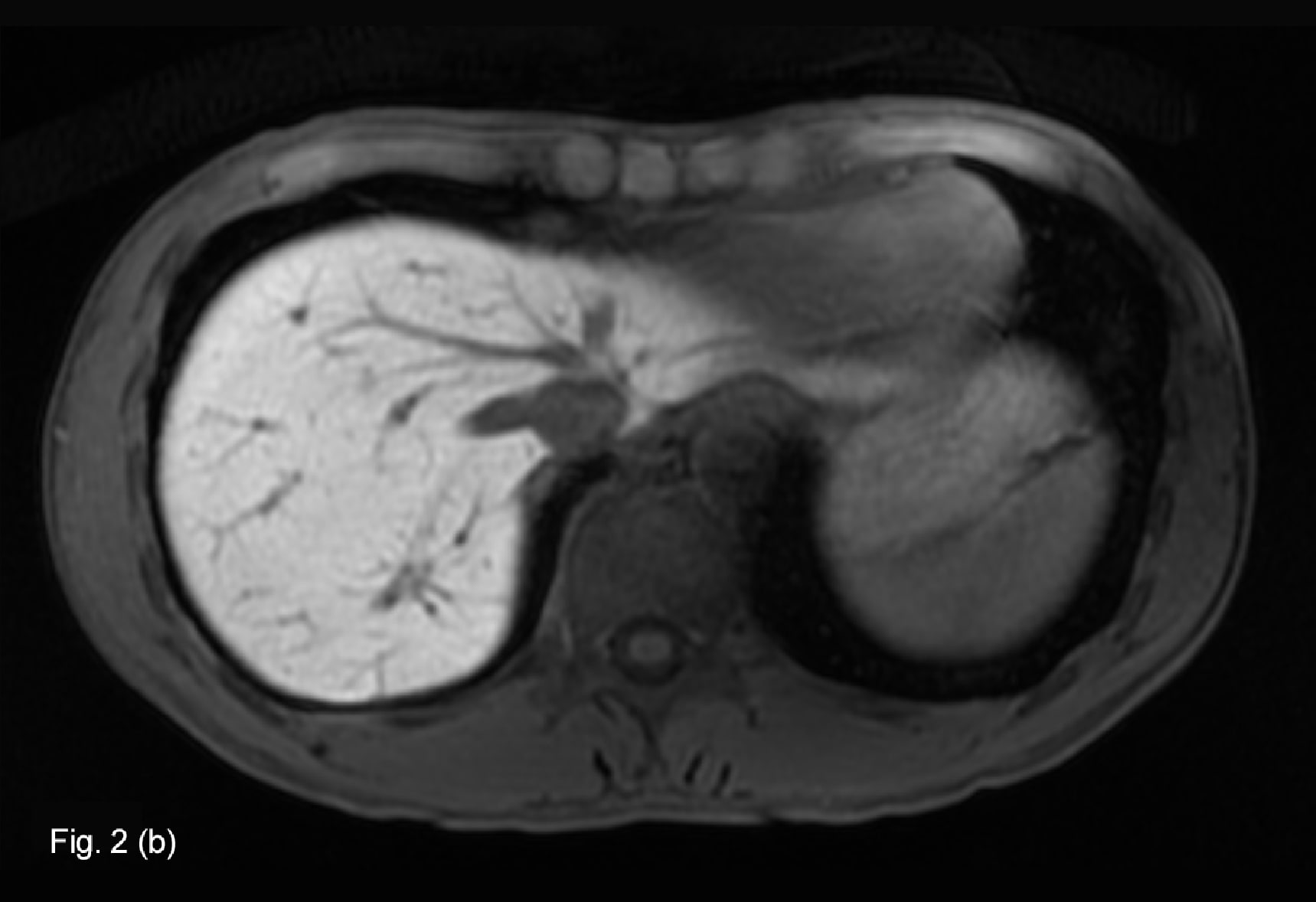
EOB-MRI (a) performed at approximately the same time as contrast CT after eight cycles of Pmab + FOLFIRI chemotherapy showed the persistence of multiple hepatic metastases.
Repeated EOB-MRI (b) after one cycle of Bmab + FOLFILI chemotherapy showed the lesions to have disappeared.
Fig. 2. EOB-MRI hepatobiliary phase
Photography protocol
| Imaging type | Photography sequence | Photography duration | TE (msec) | TR (msec) | FA (deg) | Fat sat (type) | ETL (number) | P-MRI (Reduction Factor) | Holding breath (yes/no) | NEX (calculation number) |
| Dual echo | 3D-GRE(LAVA) | 20sec | Minimum (1.1 2.2) | 5.0 | 60 | ー | - | 2.0 | Yes | 1.0 |
| Contrast agent administration | ||||||||||
| Dynamic | 3D-GRE(LAVA) | 20sec | 2.0 | 4.6 | 12 | Chem SAT (Special) | - | 2.0 | Yes | 1.0 |
| DWI | EPI | 1min 48sec | Minimum (74.6msec) | effective TR (4000~7000) | ー | Chem SAT (Special) | - | 2.0 | No | 2.0 |
| T2WI | PROPELLER | 3min 28sec | 91.7 | effective TR (4000~7000) | 140 | Chem SAT (Fat) | 28 | ー | No | 1.0 |
| Hepatobiliary phase | 3D-GRE(LAVA) | 18sec | 1.9 | 4.1 | 12 | Chem SAT (Special) | - | 2.0 | Yes | 1.0 |
| Hepatobiliary phase Cor | 3D-GRE(LAVA) | 18sec | 1.9 | 4.1 | 12 | Chem SAT (Special) | - | 2.0 | Yes | 1.0 |
| Imaging type | k-space | In-plane resolution (mm) | Slice thickness (mm) | FOV (mm) | Rectangular FOV(%) | Phase direction (step number) | Read direction (matrix number) | Slice Gap (mm) | Slice number |
| Dual echo | sequential | 1.3×1.5 | 4.0 | 380 | 80 | 256 | 288 | 2.0 | 50 |
| Contrast agent administration | |||||||||
| Dynamic | sequential | 1.3×1.5 | 4.0 | 380 | 80 | 256 | 288 | ー | 50 (using ZIP) |
| DWI | sequential | 2.7×2.4 | 8.0 | 380 | 100 | 160 | 140 | 2.0 | 20 |
| T2WI | radial | 1.3×1.3 | 8.0 | 380 | ー | 288 | 288 | 2.0 | 20 |
| Hepatobiliary phase | sequential | 1.3×1.5 | 4.0 | 380 | 80 | 256 | 288 | ー | 50 (using ZIP) |
| Hepatobiliary phase Cor | sequential | 1.3×1.5 | 4.0 | 380 | 80 | 256 | 288 | ー | 50 (using ZIP) |
Devices used and contrast conditions
| MRI device | Signa Architect |
| Automatic injection device | Sonic Shot 7 |
| Workstation | ー |
| Contrast conditions | Dose (mL) | Administration rate (mL/s) | Photography timing | |
| Gadoxetate disodium(Gd-EOB-DTPA) | 0.1mL/kg | 10-s injection | Initiation when the contrast agent reached the left ventricle (approximately 30 s, approxi-mately 70 s, and approximately 135 s) | |
| Physiological saline solution for flushing | 30mL | Same speed as contrast agent |
Usefulness of Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI with this patient
The frequency of elimination of colorectal cancer hepatic metastases is increasing with progress in chemotherapy, but such metastases are known to recur frequently after an evaluation of CR has been made by CT(1). In connection with colorectal cancer hepatic metastases after chemotherapy, hepatic fat deposition is known to occur as a result of irinotecan and 5-FU administration, and this is a factor in the decrease in contrast between the background hepatic parenchyma and the lesion, often leading to underestimation in the context of lesion detection and size evaluation. For confirming the elimination of lesions, it has been reported that hepatobiliary-phase imaging using EOB-MRI is superior to contrast CT(2).
With the present patient, contrast CR was considered to show CR, but a residual lesion was clearly shown by EOB hepatobiliary-phase imaging. Additional treatment was then provided, after which repeated EOB-MRI confirmed elimination of this lesion.
- Benoist S, Brouquet A, Penna C, et al. Complete response of colorectal liver metastases after chemotherapy: does it mean cure?. J Clin Oncol. 2006;24(24):3939-3945.
- Park MJ, Hong N, Han K, et al. Use of Imaging to Predict Complete Response of Colorectal Liver Metastases after Chemotherapy: MR Imaging versus CT Imaging. Radiology. 2017 Aug;284(2):423-431.
- *The case introduced is just one clinical case, so the results are not the same as for all cases.
- *Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


