Practical report of metastatic hepatic cancer: Gastrointestinal stromal tumor (GIST) hepatic metastases
Tohoku University Hospital
Dept. of Diagnostic Radiology: Drs. Takayuki Yamada (current affiliation: Dept. of Radiology, Sendai City Hospital), Masashi Tsuda, Tadayuki Okumoto (current affiliation: Dept. of Radiology, Osaki Citizen Hospital), Shoki Takahashi
Division of Hepato-Biliary Pancreatic Surgery: Drs. Hiroki Hayashi, Tohru Onogawa, Takanori Morikawa, Michiaki Unno
DATE : 2021
GIST hepatic metastases

Patient’s background and objectives of magnetic resonance imaging (MRI)
Female, 60s.
Screening ultrasonography performed when a GIST was found in the small intestine showed a hepatic mass approximately 10 cm in diameter. Detailed examination performed at admission to hospital showed two hepatic tumors, one approximately 11 cm in diameter, extending in the liver from S4 to the anterior segment, and the other 2 cm in diameter, in S7. Fluorodeoxyglucose positron emission tomography (FDG-PET) of the larger tumor then showed accumulation, with a maximum standardized uptake value (SUVmax) of approximately 15. These tumors were then treated by expanded right hepatic lobectomy, and the diagnosis made was GIST metastasis. Subsequently, two masses close to the resection locus were identified by computed tomography (CT) during monitoring of progression, but FDG-PET performed approximately 3 months later did not clearly show FDG accumulation, so monitoring of progression was continued. However, CT performed after a further 3 months showed an increase in the diameter of the mass, so MRI using Gadoxetate disodium(Gd-EOB-DTPA) was performed approximately 5 weeks later in order to determine whether the mass close to the resection locus was a metastatic lesion, and whether any other metastatic lesions were present.
This case study is based on real events and is intended for educational and illustrative purposes only.
CT images

a) Portal phase

b) Portal phase

c) Portal phase
Multidetector CT
A mass lesion showing low absorption was found to the lateral side of the staple close to the resection locus (b: red arrow).
A second mass lesion showing low absorption was found to the cranial side of the first (a: red arrow). In the portal phase, a faint, low-absorption lesion (c: blue arrow) was found at the abdominal end of S3 in the lateral segment of the hepatic left lobe, separated from the other lesions. The lesion in S3 could be identified by reinterpretation, after MRI, but it was difficult to recognize, and could not be identified at all in the other phases (pre-contrast, arterial, and equilibrium).
MRI images

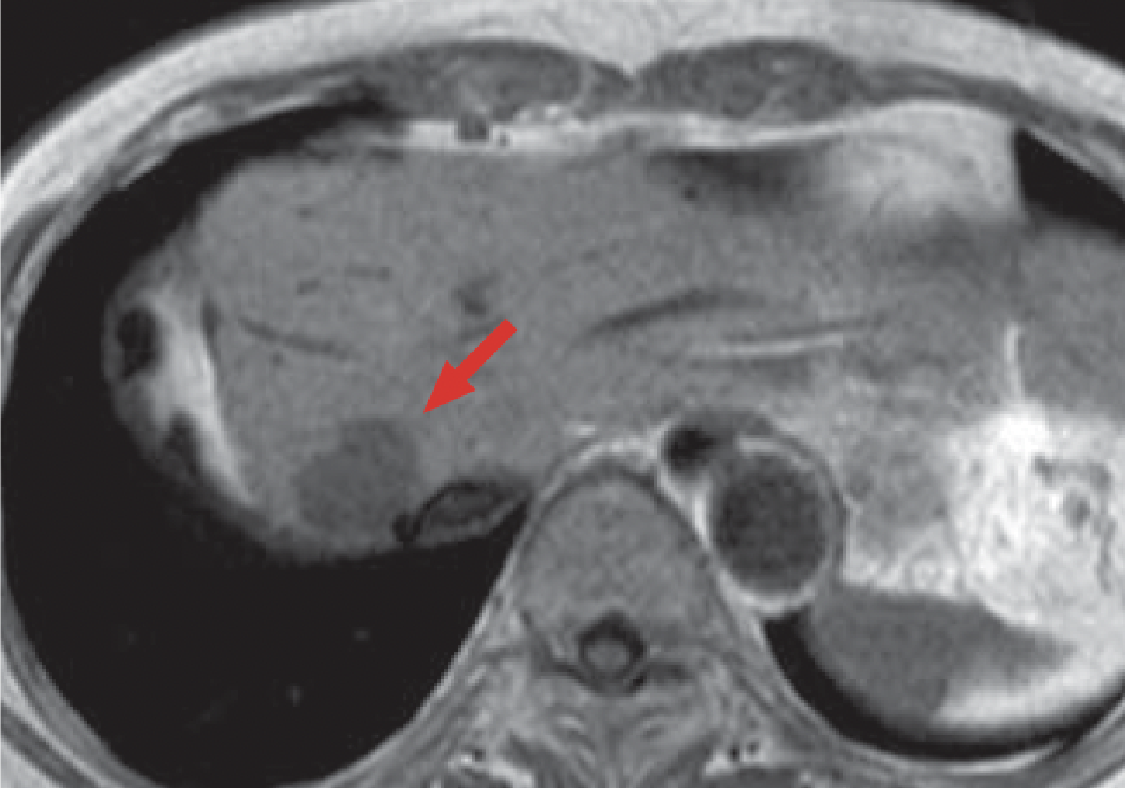
d) T2-weighted imaging

g) Pre-contrast, T1-weighted imaging

e) T2-weighted imaging
h) Pre-contrast, T1-weighted imaging

f) T2-weighted imaging

i) Pre-contrast, T1-weighted imaging
MRI
Two mass lesions of different sizes were found close to the resection locus (red arrow).
In addition, one small mass lesion was found at the abdominal end of S3, separated from the other two lesions (blue arrow).
All three lesions gave homogeneous high signals in T2-weighted imaging (d, e, f), and low signals in T1-weighted imaging (g, h, i).

j) Arterial phase

m) Hepatobiliary phase

k) Arterial phase

n) Hepatobiliary phase

l) Arterial phase

o) Hepatobiliary phase
Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI
In the arterial phase (j, k, l), contrast enhancement in the two masses close to the resection locus was weak (red arrow), and the mass lesion in S3 was visualized as a ring shape (blue arrow).
In the hepatobiliary phase (m, n, o), all three masses showed distinct contrast loss (red and blue arrows).
These three mass lesions were judged to be hypovascular tumors, and were suspected of being metastases.
Overview of hepatic diagnostic imaging and treatment performed with this patient

Impact of Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI on diagnosis
With the present patient, CT showed a relatively large lesion close to the resection locus, and another lesion, adjacent to that one. However, the small lesion in S3 in the lateral segment of the left hepatic lobe was very difficult to detect, and this lesion could not be found using CT alone, so the procedure may have been completed with resection of the S4 locus only. The lesion in S3 was identified using Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI, enabling the three lesions to be resected simultaneously. Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI is considered to be useful for selecting surgical techniques for resection of metastatic lesions.
The hepatobiliary phase of Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI showed liver-specific contrast enhancement, and in this phase 3D gradient-echo imaging was feasible, as was accurate judgment of lesion positions using thin slices. However, in the hepatobiliary phase, but not other phases, apart from metastatic lesions, cysts and other benign lesions, and, depending upon lesion size, hemangioma, show contrast loss, making qualitative diagnosis difficult. Nevertheless, it is possible to differentiate between these lesions by assessing contrast enhancement (hemodynamic information) on the basis of dynamic imaging.
Two advantages of use of Gadoxetate disodium(Gd-EOB-DTPA) are considered to be that (i) dynamic imaging enables verification of hemodynamic information about lesions, which is difficult to achieve using superparamagnetic iron oxide (SPIO) contrast agents; and (ii) detailed observation can be achieved more readily by fat-suppressed, 3D, T1-weighted imaging than by SPIO contrast MRI T2-weighted imaging, .
Impact of Gadoxetate disodium(Gd-EOB-DTPA) (gadoxetate disodium) contrast MRI on treatment
The present patient had a GIST, in the small intestine, and small intestinal resection was performed in April 2007, followed by expanded right hepatic lobectomy in June 2007, and then monitoring of progression on an out-patient basis without adjuvant chemotherapy. In June 2008, CT showed two low-absorption regions, considered to be tumor recurrence, in the remaining liver, and surgery was scheduled. However, it was then demonstrated by Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI that three lesions were in fact present.
In particular, the visualization of this tumor in the hepatobiliary phase was excellent, and lesions that were with difficulty visualized using CT and conventional MRI were visualized clearly. Retrospective reassessment of the CT findings showed that three lesions could be identified, albeit with difficulty. However, if Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI is not performed, there is the potential for tumors to be overlooked, and surgery thus to be left incomplete. In addition, there have been other patients with whom hepatic tumors judged to be single foci on the basis of CT were later clearly shown to be multiple.
In the case of patients with intrahepatic neoplastic lesions, at Tohoku University Hospital, Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI is considered to be essential for successfully performing surgery so that none of the tumor remains.
- *The case introduced is just one clinical case, so the results are not the same as for all cases.
- *Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


