Evaluation of cTACE and DEB-TACE therapeutic efficacy using Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI (2)
Fukui-ken Saiseikai Hospital
Dept. of Diagnostic Radiology
Dr. Shiro Miyayama
DATE : 2021
Introduction
In Japan, the mainstream form of hepatic arterial chemoembolization (TACE) is conventional TACE (cTACE), in which lipiodol and a gelatin sponge (GS) are used. However, drug-eluting beads (DEBs) were introduced at the beginning of 2014. The basic principle of DEB-TACE is that blood vessels in and close to tumors are filled with granules that slowly release anticancer drugs, resulting in both ischemia and antitumor effects, and thus necrosis of the tumor. The therapeutic outcome has been evaluated as similar to that with cTACE, but DEB-TACE is expected to be effective for treating patients with advanced tumors and/or low hepatic functional reserve, and various studies have been performed at different facilities.
On the other hand, in the case of patients unresponsive to TACE, it is necessary to promptly decide upon the second-line therapeutic method, such as molecular-targeted drugs, and more accurate evaluation of therapeutic efficacy is therefore needed. Computed tomography (CT) and Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI (EOB-MRI) are used to evaluate therapeutic effects after TACE, but evaluation after cTACE is sometimes hindered by the effects of lipiodol accumulated inside the tumor. In addition, it is sometimes difficult to distinguish minute residual tumors from treatment-related inflammation after DEB-TACE. In principle, the present author performs CT and EOB-MRI alternately at 2- to 3-month intervals after TACE, but evaluation by EOB-MRI is also performed if recurrence or persistence is suggested, but cannot be confirmed, by CT. Two patients with whom EOB-MRI was used for follow-up observation after TACE are presented below.


Magnetic resonance imaging (MRI) method using Gadoxetate disodium(Gd-EOB-DTPA)-contrast MRI
Sequence and sequence parameters
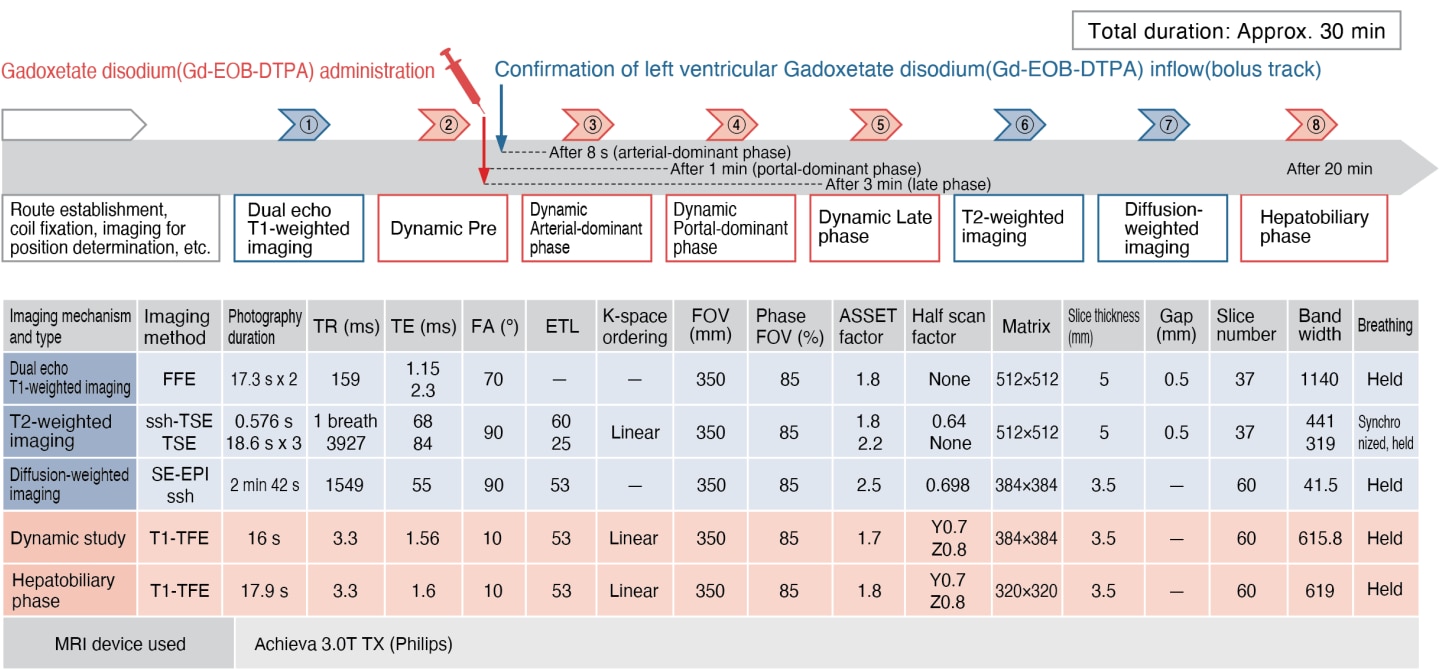
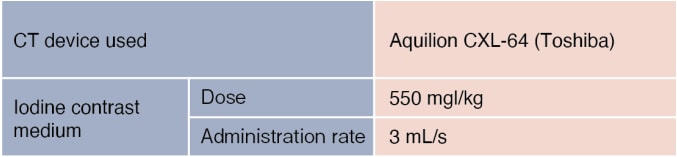
Contrast agent and administration method
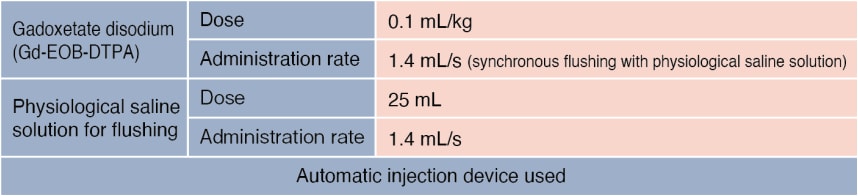
CT method
Case presentation

Patient’s background and objectives of MRI
Male, 80s
At a different hospital, CT was performed as a thorough examination of arteriosclerosis obliterans, and a tumor was found in the liver, so the patient was referred to the author’s hospital.

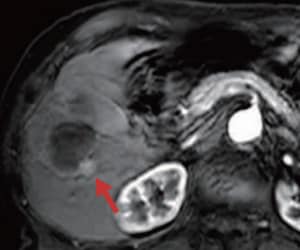
Simple CT (a)
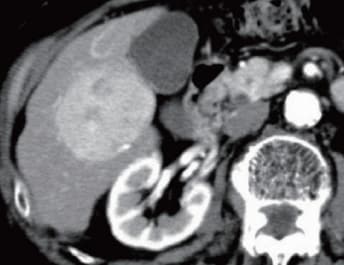
S6: Arterial-dominant phase (b)

S6: Equilibrium phase (c)
DSA (d)
CT and digital subtraction angiography (DSA) imaging
CT and DSA findings
Simple CT (a) showed low absorption in S6, and a tumor 6.3 cm in diameter was found, showing early-stage dark staining in the arterial-dominant phase (b), and wash-out in the equilibrium phase (c). DSA showed distinct dark staining of the tumor (d).
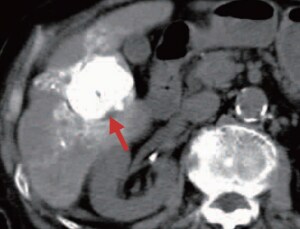
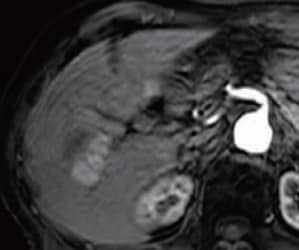
Simple CT (e)
CT during the treatment course
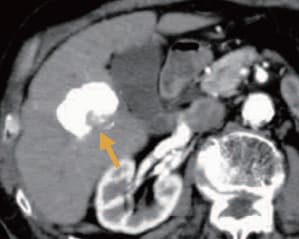
Arterial-dominant phase (f)
CT during the treatment course
Portal-dominant phase (g) *
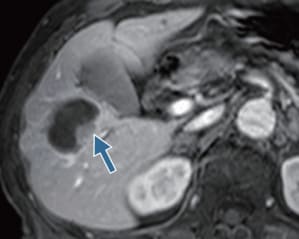
EOB-MRI during the treatment course

Hepatobiliary phase (h)
EOB-MRI during the treatment course
CT and EOB-MRI findings
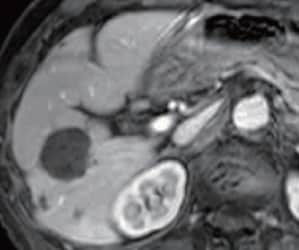
The cancer was unifocal, but, because the patient was elderly, cTACE was performed, using a suspension of 6 mL of lipiodol, 30 mg of epirubicin, and 6 mg of mitomycin C, and GS. Simple CT (e) after 1 week showed high-concentration lipiodol accumulation in the tumor, but the therapeutic safety margin in the dorsal region was insufficient (red arrow). The dynamic CT arterial-dominant phase (f) after 4 months suggested recurrence on the dorsal side of the tumor (yellow arrow), so EOB-MRI was performed. Artifacts were generated in the arterial-dominant phase, making evaluation difficult, but in the portal-dominant phase (g) and hepatobiliary phase (h) distinct recurrence was found (blue arrow), so cTACE was performed, using a suspension of 3 mL of lipiodol, 20 mg of epirubicin, and 4 mg of mitomycin C, and GS.
Arterial-dominant phase (i)*
Arterial-dominant phase (j)
EOB-MRI during the treatment course
EOB-MRI findings
In the EOB-MRI arterial dominant phase (i) after 18 months, recurrence was found at the same locus as the initial tumor (red arrow), so cTACE was performed again, using a suspension of 4 mL of lipiodol, 20 mg of epirubicin, and 4 mg of mitomycin C, and GS. However, artifacts were markedly noticeable in the EOB-MRI arterial-dominant phase (j) after 2 years, indicating recurrence at the same locus.
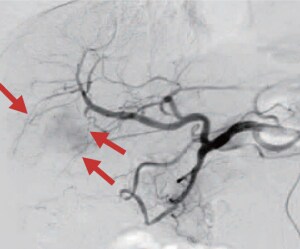
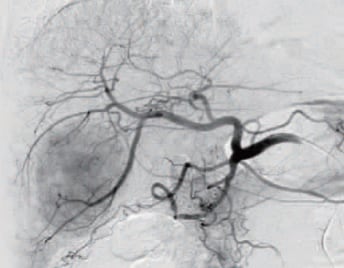
DSA (k)
DSA imaging at the time of DEB-TACE
DSA findings
cTACE was followed by repeated local recurrence, so DEB-TACE was judged to be indicated, and DEBs were prepared in the same manner as for Case Presentation 1. DSA (k) of the common hepatic artery showed dark staining of the tumor, and DEB-TACE was performed from one branch of A5 and two branches of A6 (red arrows)(0.8 mg of DEBs used).
A small quantity of GS was added for embolization of one branch of A6.

Portal-dominant phase (l)
EOB-MRI imaging after DEB-TACE
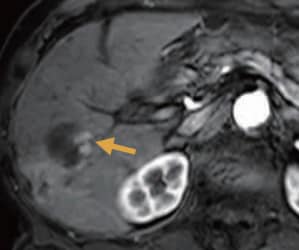
Arterial-dominant phase (m)*
EOB-MRI imaging after DEB-TACE

Simple CT (n)*
CT imaging after DEB-TACE
Portal-dominant phase (o)
EOB-MRI imaging after DEB-TACE
CT and EOB-MRI findings
In the arterial-dominant phase of EOB-MRI after 3 months, artifacts were generated, making evaluation difficult, but linear staining was found in the tumor marginal region in the portal-dominant phase (l; red arrow), and in the EOB-MRI arterial-dominant phase after 5 months (m) the tumor was found to have expanded (yellow arrow), so recurrence was diagnosed, and three new lesions were also found. cTACE was performed using a suspension containing 4 mL of lipiodol, 20 mg of epirubicin, and 4 mg of mitomycin C, and GS, and simple CT (n) 1 week later showed high-concentration lipiodol accumulation at the recurrence locus and in the surrounding hepatic parenchyma. In the EOB-MRI arterial-dominant phase after 3 months (2 years 8 months after the initial treatment), artifacts made evaluation difficult, but on the basis of the portal-dominant phase (o) there was judged to be no recurrence.
Usefulness of EOB-MRI diagnostic imaging results with this patient
With the present patient, artifacts were generated several times during the EOB-MRI arterial-dominant phase, making evaluation difficult. However, in the portal-dominant phase, the recurrent tumor showed a lower signal than the surrounding hepatic tissue, with staining in the marginal region, and even in the hepatobiliary phase there was a difference in signal intensity between the necrotic and viable portions, so recurrence was diagnosed without difficulty. When dark staining is found in the tumor and marginal region after DEB-TACE, it is possible that a residual tumor is present, so considerable care must be taken. In addition, in relation to these findings, it is necessary to distinguish between (i) a peritumoral arterioportal shunt associated with an embolism; and (ii) inflammation.
Precautions relating to administration
Administration to elderly patients
Elderly patients generally show depressed physiological function, and administration must be performed with care, and with sufficient monitoring of the patient’s condition.
- * The case introduced is just one clinical case, so the results are not the same as for all cases.
- * Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


