Hepatocellular carcinoma intrahepatic metastases and multicentric lesions
University of Yamanashi Hospital
Faculty of Medicine,
First Dept. of Surgery: Drs. Masanori Matsuda, Hideki Fujii
Dept. of Radiology: Drs. Tomoaki Ichikawa, Katsuhiro Sano
DATE : 2021
Patient’s background and objectives of magnetic resonance imaging (MRI)
Male, 70s.
Multiple hepatocellular carcinoma (HCC), consisting of intrahepatic metastases and multicentric, early-stage HCC.
During observation of the progression of chronic hepatitis C, a local physician found a hepatic mass by abdominal ultrasonography, and referred the patient to the authors’ hospital for thorough examination and treatment.The patient was admitted, and the test results at that time were as follows: HCV antibody: positive; HBs antigen: negative; HBs antibody: positive; HBc antibody: positive; indocyanine green retention rate at 15 min: 28.2%; liver damage severity: B; Child-Pugh score: 6; and Child-Pugh class: A.The tumor-marker results were as follows: α-fetoprotein: 42.2 ng/mL, indicating an increase; L3 fraction: 1.5%; and PIVKA-II: 30 mAU/mL.
Previous medical history: Surgery for appendicitis at the age of 37, and chronic hepatitis C.
Patient’s background: No history of blood transfusion, but histories of excessive alcohol consumption and smoking.
Physical findings: Anemia, jaundice, no encephalopathy.No abnormal thoracic findings.A surgery scar was present in the right lower abdomen.The center of the right hypochondrial region of the liver was palpable to two fingerbreadths, but the spleen was not palpable.No ascites was present.
Imaging parameters and contrast agent administration method
Sequence and sequence parameters
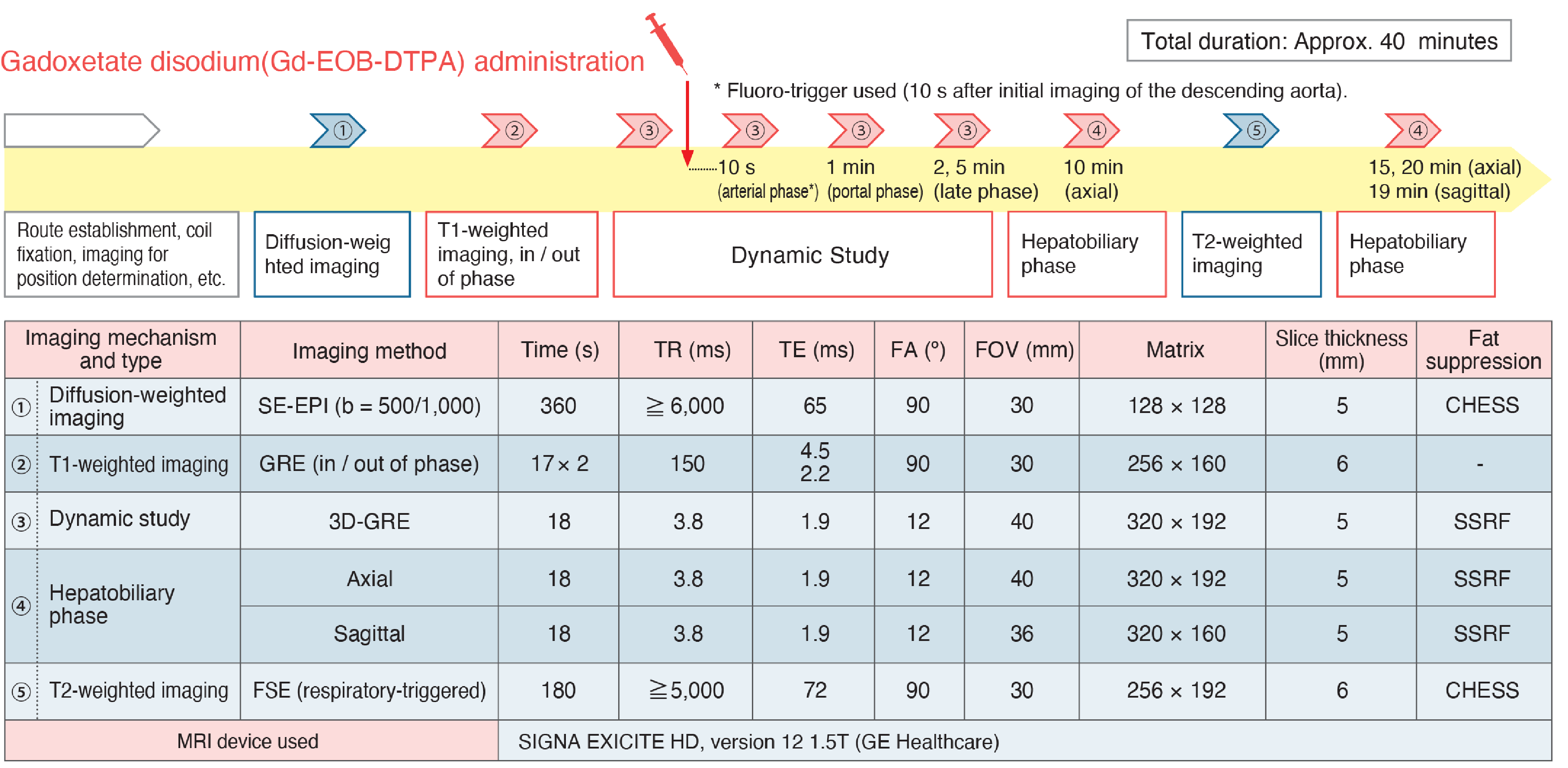
Contrast agent and administration method
Cautions and supplements
Dose administered: Stipulated dose
Injection rate: Recommended rate is 1.0 to 2.0 mL/s.
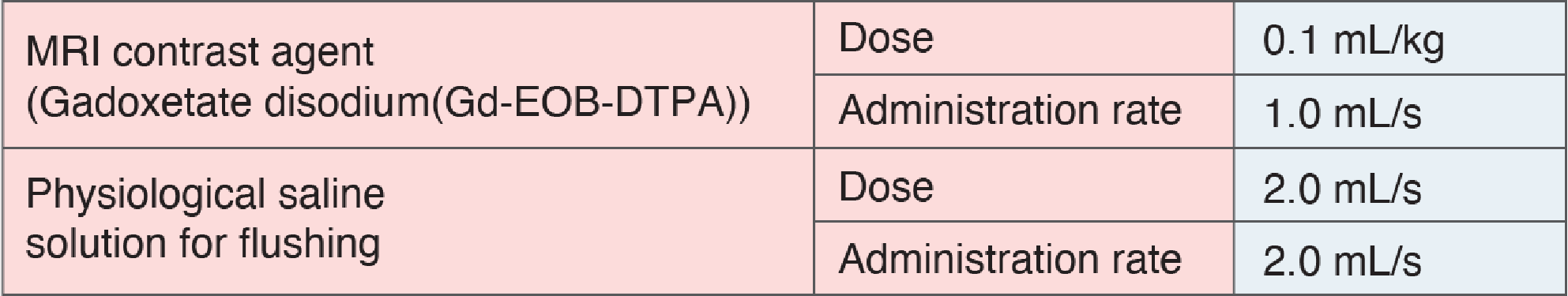
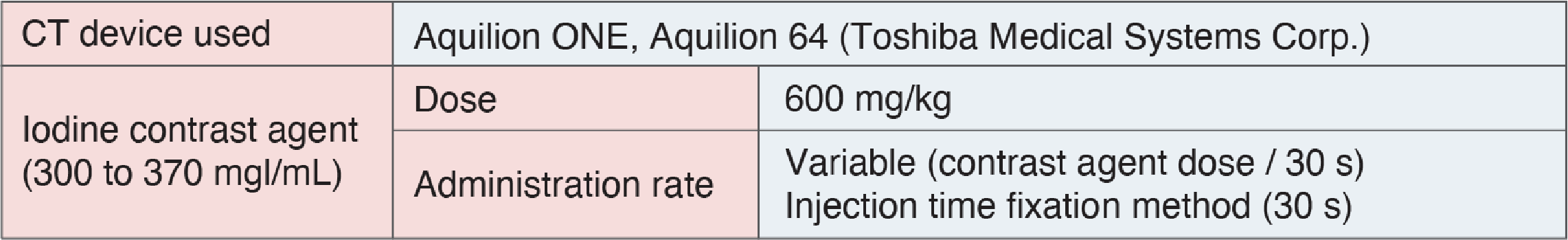
For reference: Contrast computed tomography (CT) standard protocol
Imaging findings
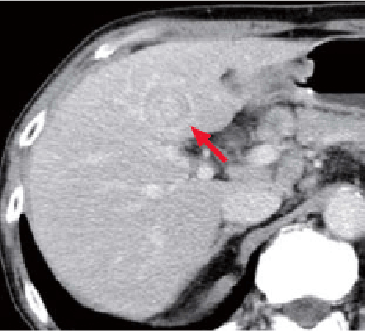
a) Arterial phase
b) Equilibrium phase
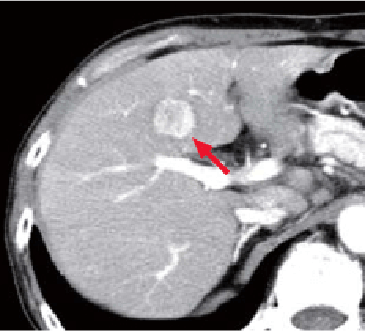
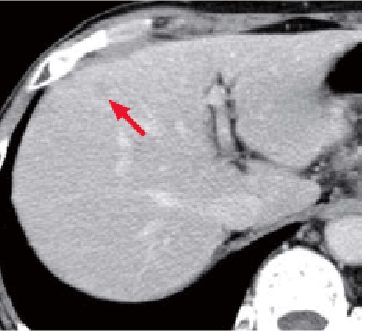
Multidetector CT (liver S4)
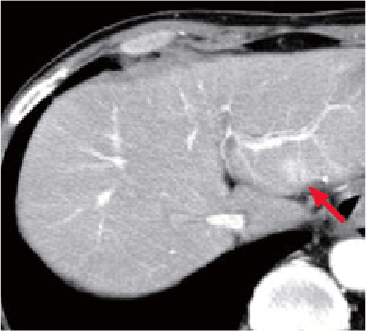
c) Arterial phase
d) Equilibrium phase
MDCT (liver S2)
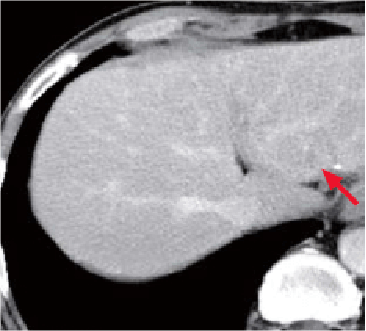
e) Arterial phase
f) Equilibrium phase
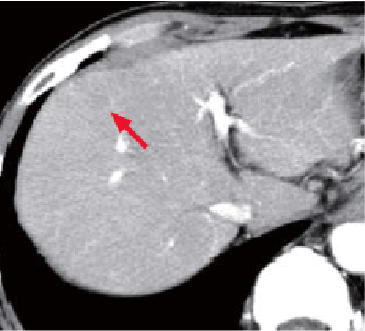
MDCT (liver S4/8)
CT findings
Nodules (→) found in the liver S4 and S2 showed dark staining in the arterial phase (a, c), and wash-out in the equilibrium phase (b, d). The nodule diameters were 2.5 cm in liver S4, and 1.4 cm in liver S2.
In addition, below the S4/8 dome in the liver, there was a nodule (→) that was 1.0 cm in diameter, and showed low absorption in both phases (e, f).
g) Pre-contrast, T1-weighted imaging, in phase
i) T2-weighted imaging
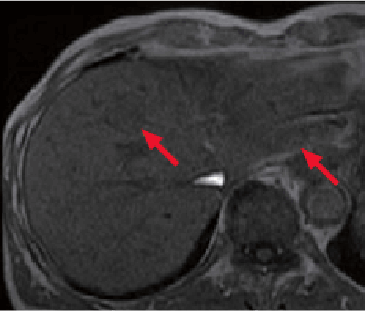
MRI
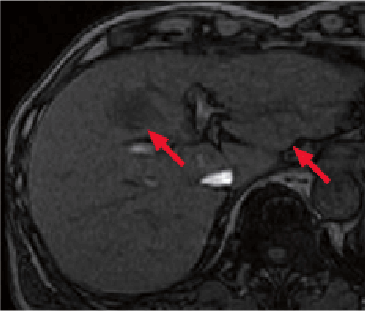
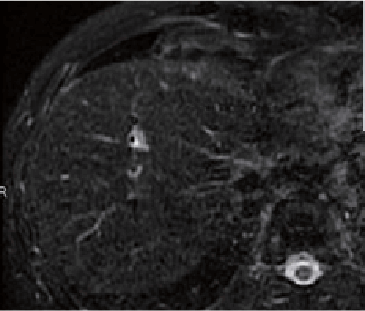
k) Arterial phase
Gadoxetate disodium
(Gd-EOB-DTPA) contrast MRI
h) Pre-contrast, T1-weighted imaging, out of phase
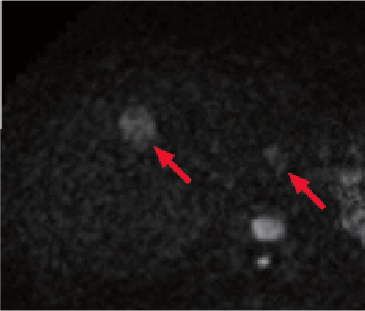
j) Diffusion-weighted imaging (b value = 1000 s/mm2)
MRI
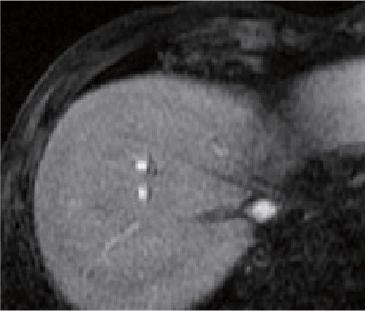
l) Hepatobiliary phase
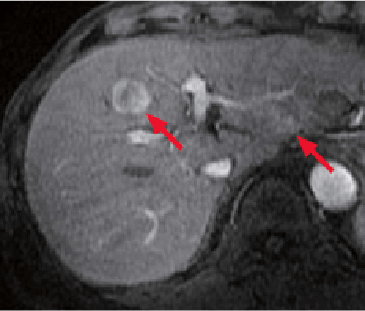
Gadoxetate disodium
(Gd-EOB-DTPA) contrast MRI
MRI findings
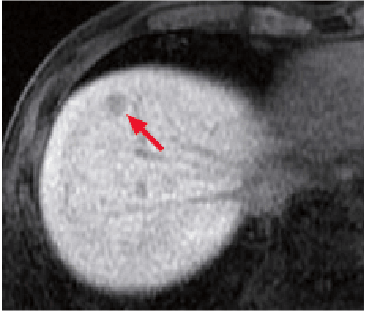
In liver S4 and S2, nodules (→) were found that showed low signals in T1-weighted imaging (g, h), and high signals in fat-suppressed T2-weighted imaging (i), and diffusion-weighted imaging (b value = 1000 s/mm2; j).
With Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI, these nodules (→) showed high signals in the arterial phase (k), and low signals in the hepatobiliary phase (l). The diameters were 2.5 cm for the S4 nodule, and 1.4 cm for the S2 nodule.
On the basis of these findings, the S4 and S2 nodules (→) were diagnosed as moderately to highly differentiated HCC.
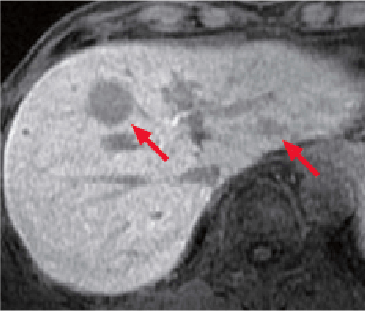
m) Pre-contrast, T1-weighted image, in phase
o) T2-weighted image
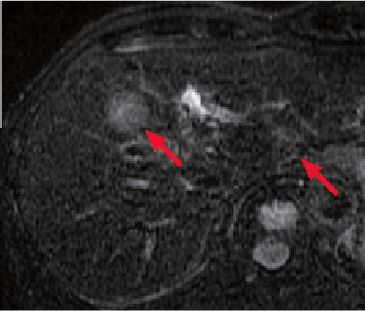
MRI
q) Arterial phase
Gadoxetate disodium
(Gd-EOB-DTPA) contrast MRI
n) Pre-contrast, T1-weighted image, out of phase
p) Diffusion-weighted image (b value = 1000 s/mm2)
MRI
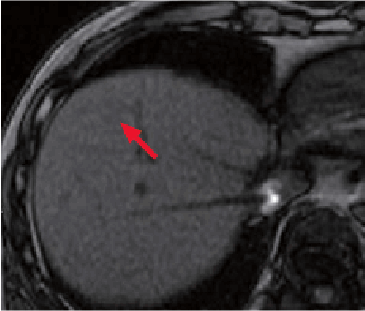
r) Hepatobiliary phase
Gadoxetate disodium
(Gd-EOB-DTPA) contrast MRI
MRI findings
Below the liver S4/8 dome, with T1-weighted imaging a nodule (→) was found that showed a faint high signal in phase (m), and part of which showed a low signal out of phase (n). It was suggested that part of this nodule was a mass containing fat.
No images of this nodule were obtained by fat-suppressed, T2-weighted imaging (o), or diffusion-weighted imaging (p).
In the hepatobiliary phase (r) of Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI, a nodule (→) 1.0 cm in diameter was found that was fixed as a distinct low-signal nodule.
This nodule was not found pre-contrast (images not shown) or arterial phase (q), and was suggested to be a hypovascular lesion.
In summary, the small nodule (→) below the S4/8 dome was diagnosed as highly differentiated HCC, with a different degree of differentiation from the principal tumor in liver S4.
Course of treatment
On the basis of diagnostic imaging, the preoperative diagnoses made were advanced HCC 2.5 cm in diameter in hepatic medial segment S4, intrahepatic metastasis in hepatic lateral segment S2, and multicentric, highly differentiated HCC in S4/8. The optimal surgical procedures for such lesions are left hepatectomy and anterior partial hepatectomy, but, taking hepatic function into consideration, the procedures performed were medial segmentectomy, partial S2 resection, partial S4/8 resection, and cholecystectomy. Postoperative progression was favorable, and the patient was discharged from hospital on day 14 of treatment.
Pathological findings
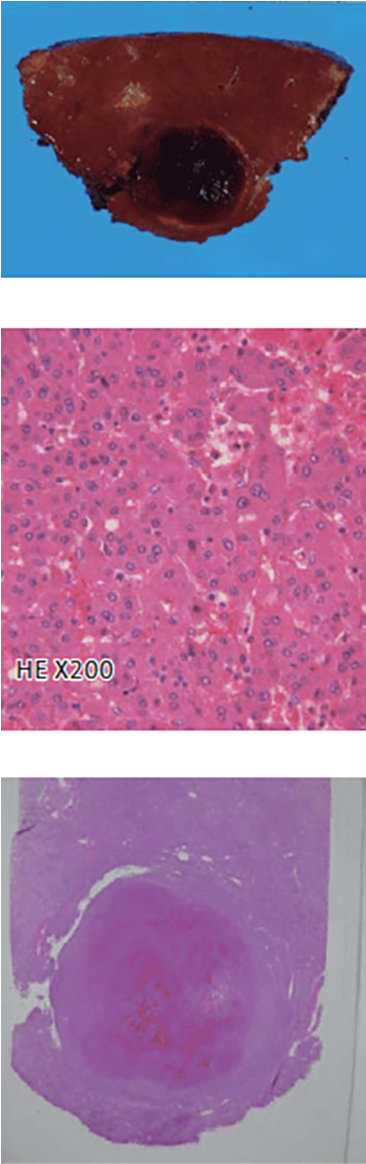
s) Liver S4
t) Liver S2
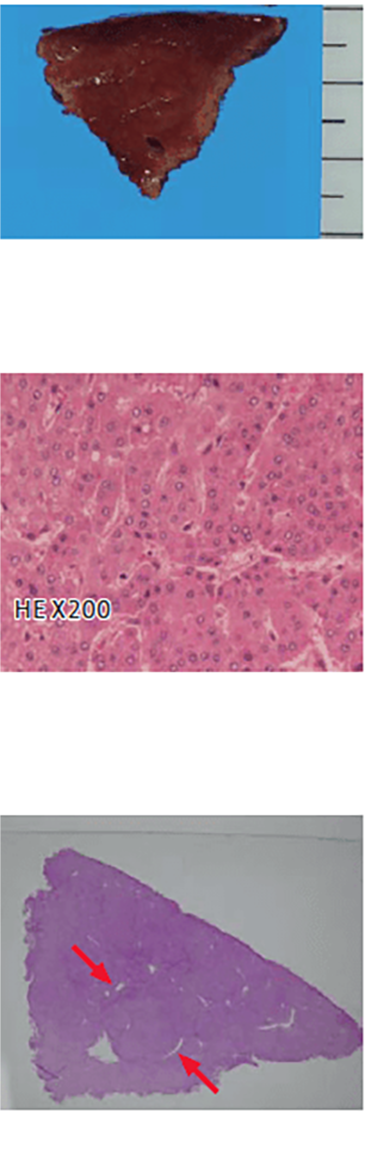
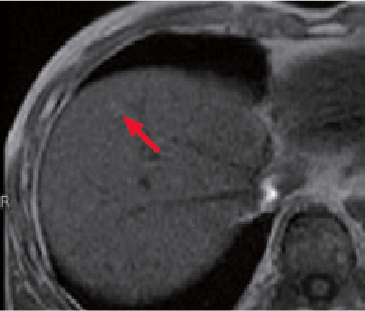
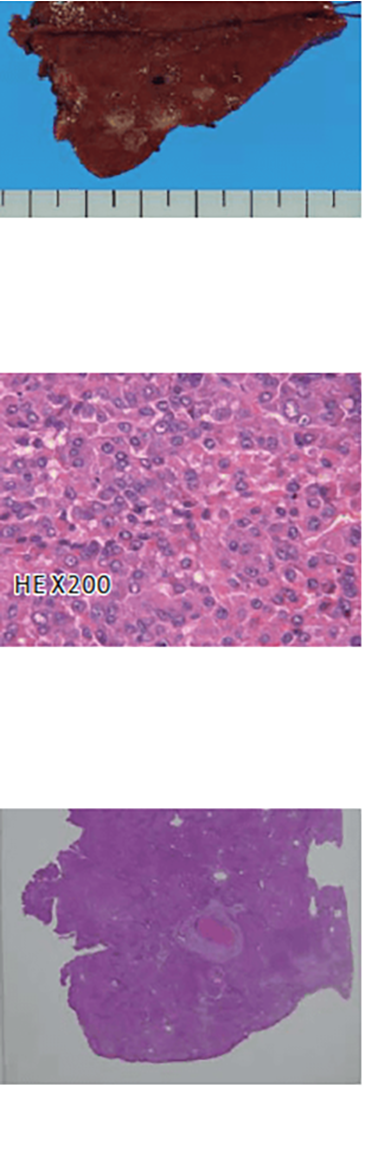
u) Liver S4/8
pathology specimen
Pathological findings
The principal tumor (s) in liver S4 was a simple nodular tumor with a capsule and a maximum diameter of 2.5 cm, associated with hemorrhage in part of the tumor.
In histological terms, it was moderately differentiated HCC consisting of a medium to large cord-like structure, and a highly differentiated HCC component was found in part of the marginal region.
An accessory tumor (t) in liver S2 was visually observable as a yellow-white nodule 0.4 cm in diameter, and in histological terms it was moderately differentiated HCC similar to the principal tumor, with a minute portal vein tumor thrombus and other thrombogenesis in the surrounding region.
The tumor (u) in liver S4/8 was a lesion (→) of small nodular type with indistinct margin (the margin was indistinct in visual assessment), 1.0 cm in diameter, that was mostly found to be a similar color to the surrounding hepatic tissue in visual assessment, but with a yellow part, and with some of the hepatic structure remaining inside the tumor.
In histological terms, it was highly differentiated HCC, with a fine cord-like structure and no capsule formation, in part of which fatty changes, a pseudotubular structure, and interstitial tissue tumor cell infiltration were found.
It was diagnosed as early-stage, multicentric HCC.
Summary
Gadoxetate disodium(Gd-EOB-DTPA) MRI has a higher detection effectiveness for early-stage HCC than dynamic CT, CTHA, or CTAP, and is a highly useful modality for diagnosis of multicentric HCC. HCC has a high rate of intrahepatic metastasis, and also gives rise to both synchronous and heterochronous multicentric cancer. In multiple HCC patients, if imaging diagnosis shows any accessory tumors to be either intrahepatic metastases or multicentric cancer, this is probably useful for making decisions about treatment methods. In other words, although radical resection is difficult in the case of patients with multiple HCC due to intrahepatic metastases consistently outside the resectable range, in the case of patients with multiple HCC due to multicentric cancer, radical resection is sometimes feasible. In addition, although resection is not indicated for patients with early-stage, hypovascular HCC alone, if a preoperative diagnosis of early-stage liver cancer is made, it is feasible to treat early-stage ischemic HCC by resection or ablation at the same time as resection of the advanced HCC, which can be expected to contribute to prevention of post-hepatectomy recurrence.
According to General Rules for the Clinical and Pathological Study of Primary Liver Cancer, if multiple HCC lesions are found, and the cancer is early-stage HCC with atypical nodules and maintenance of existing hepatic structure, and/or HCC with highly differentiated cancer tissue at the margins of poorly or moderately differentiated cancer tissue, it is strongly suggested that the cancer is growing at the primary focus, and such lesions are considered to constitute multicentric cancer. On the other hand, a lesion that meets one of the following criteria is taken to be an intrahepatic metastasis: (i) a cancer lesion that is considered to have developed as or from a portal vein tumor thrombus; (ii) in the case of a group of cancer lesions, lesions are most numerous closest to the largest tumor, becoming less numerous with distance from that tumor; and (iii) in the case of a solitary cancer lesion, it is close to a large tumor, is clearly smaller than that tumor, and in terms of histiotype is similar to that tumor or less differentiated.
For diagnostic imaging of multicentric HCC, it is necessary to either diagnose highly differentiated early-stage HCC, or detect a highly differentiated cancer component in the tissue surrounding the cancer nodule. Clinical data from the authors’ hospital clearly shows that the detection effectiveness of Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI for early-stage HCC is higher than that of dynamic CT, CTHA, or CTAP. In addition, the authors have a great deal of experience with patients with whom Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI clearly detected highly differentiated cancer components in the cancer nodular circumferential region, and Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI is therefore considered to be an extremely useful modality for diagnostic imaging of multicentric HCC.
Precautions relating to administration
Administration to elderly patients
Elderly patients generally show depressed physiological function, so administration must be performed with care, and with sufficient monitoring of the patient’s condition.
- *The case introduced is just one clinical case, so the results are not the same as for all cases.
- *Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


