The usefulness of EOB-MRI in the detection of the high-risk nodule before showing vascularity of hepatocellular carcinoma
Taipei Veterans General Hospital
Chien-An Liu
Division of abdominal imaging, Department of Radiology, Taipei Veterans General Hospital, Taipei, Taiwan.
Pei-Chang Lee
Division of Gastroenterology and Hepatology, Department of Medicine, Taipei Veterans General Hospital, Taipei, Taiwan.
DATE : 2022
Patient characteristics

Patient’s background
75 years old, Male, 88kg
Disease(s): non-hypervascular hypointense hepatocellular nodules
Patient characteristics and purpose of contrast-enhanced MRI
This 75-year-old gentleman has chronic hepatitis B and has regular imaging follow-up. His MR imaging showed cirrhotic liver with marked fibrosis and diffuse nodular regeneration. Given that heterogenous signal intensity of multiple regeneration nodules on T1-weighted image (T1WI) would hinder the detection of small hepatocellular carcinoma (HCC), EOB-MRI was chosen as the primary follow-up imaging modality.
Contrast agent used/ Dose
Gadoxetate disodium(Gd-EOB-DTPA) injection 0.1 mL/kg
Case description
During regular follow-up by the EOB-MRI imaging, a 7mm nodule was identified at segment 8 of liver. This nodule showed hypovascularity in the arterial phase and hypointensity in the hepatobiliary phase, which was indicated as a ‘‘high-risk nodule’’ or “non-hypervascular hypointense nodule (NHHN)” (Figure 1). Eight months later, this nodule grew to 1cm in diameter, and developed hypervascularization displaying a “wash-in and wash-out” typical enhancement pattern of HCC (Figure 2). Therefore, the patient underwent radiofrequency ablation (RFA) for this tumor. Complete ablation was confirmed by the follow-up MR examination (Figure 3).
Images
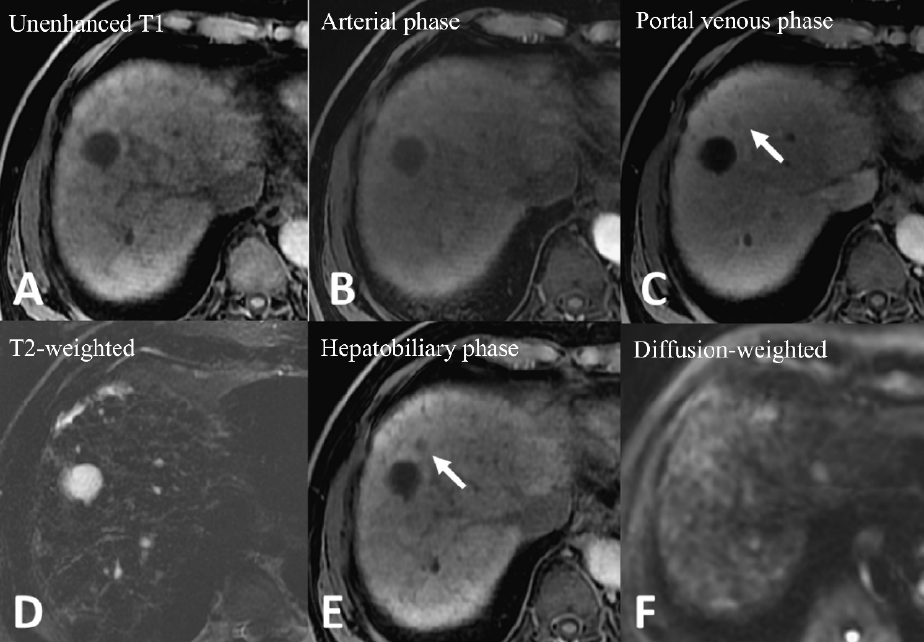
MRI showed cirrhosis and hepatic fibrosis with diffuse regenerative nodules in the liver (A). No any enhancing nodule was detected in the arterial phase (B). Portal phase images showed a 7mm hypointense nodule at segment 8 of the liver (C). This nodule displayed hypointensity in 20 minutes hepatobiliary phase (HBP) images (E) but did not show high signal intensity in T2-weighted images (T2WI) (D) or restricted diffusion (F).
Figure 1. Gd-EOB-DTPA-enhanced magnetic resonance imaging (MRI)
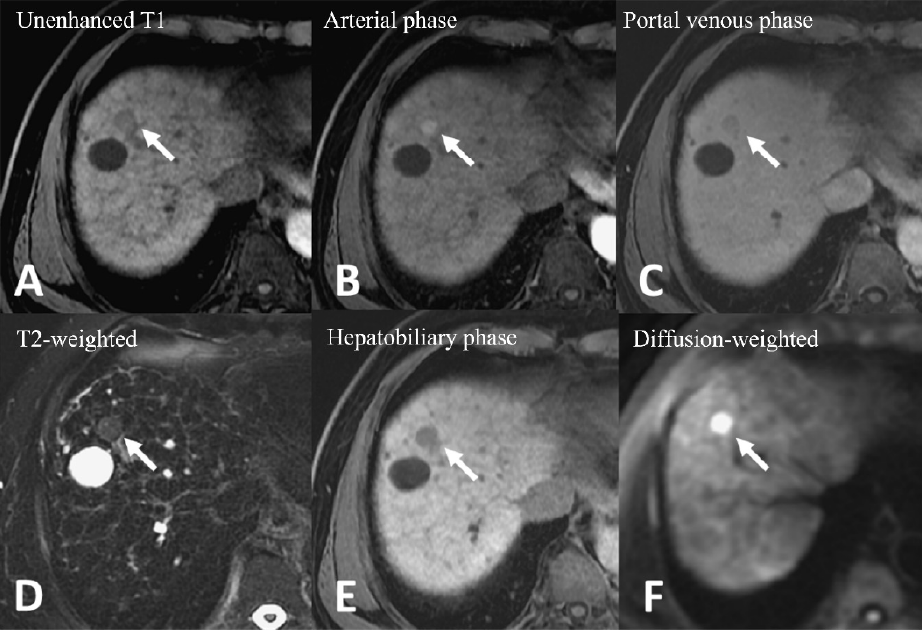
The follow-up MR images were obtained eight months after initial examination. The pre-contrast phase MR image showed a 1 cm nodule with hypointensity (A). Hypervascularization of this nodule was noted from the arterial phase image (B), and washout pattern was displayed by the delayed-phase image (C), confirming the diagnosis of HCC. This nodule showed high signal intensity on T2-weighted MR images (D), hypointensity on the HBP (E), and restricted diffusion on the diffusion-weighted image (DWI) (F).
Figure 2. Gd-EOB-DTPA–enhanced magnetic resonance imaging (MRI)
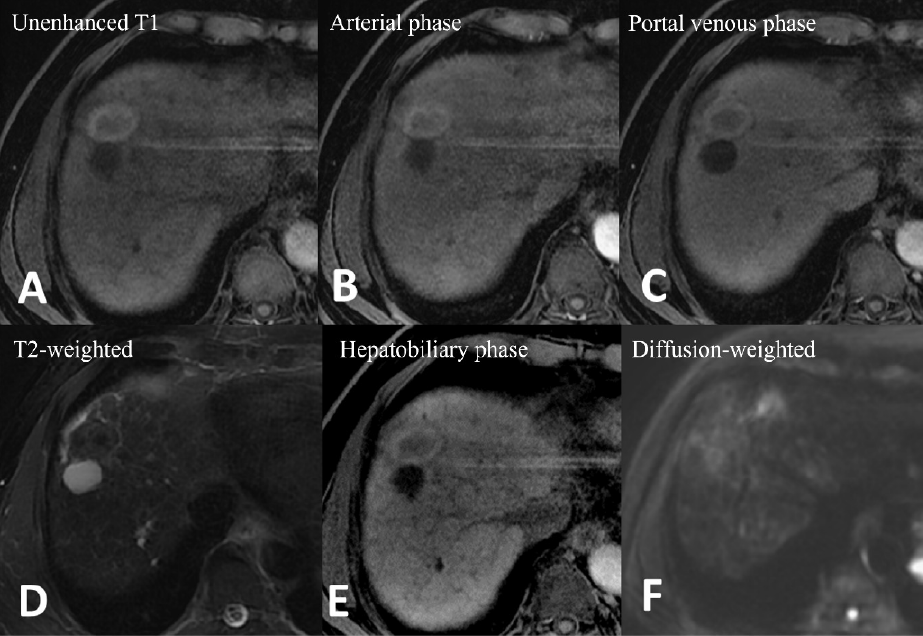
After RFA, all followed-up images confirmed complete coverage of the target tumor without viable tumor.
Figure 3. Gd-EOB-DTPA–enhanced magnetic resonance imaging (MRI)
Usefulness of contrast-enhanced MRI with Gadoxetate disodium(Gd-EOB-DTPA) in this case
The development of hepatocellular carcinoma (HCC) is a multistep process from preneoplastic lesions, including regenerative nodule (RN) and dysplastic nodule (DN), to malignant tumor. Unlike overt HCC which shows hypervascularity on the arterial phase images, RN and DN may appear hypointense, isointense, hyperintense, or mixed signal intensity on T1WI compared to the background liver, but not hypervascularity1. In high-risk patients, these hypovascular nodules may show hypointensity on the HBP of EOB-MRI, which was known as non-hypervascular hypointense nodules (NHHNs)2. These nodules could have malignant potential and are considered to be clinical precursors of HCCs3.
A meta-analysis revealed the pooled overall rate of hypervascular transformation of a NHHN was 28.2%, with 1-, 2-, and 3-year cumulative incidence rates of 18.3%, 25.2%, and 30.3%, respectively4. High SI on T2WI and restricted diffusion were known as independent predictors of transformation into hypervascular HCCs, with a median time of 8.0 months versus 62.0 months for the nodules without imaging perdictors5. Moreover, the nodular size larger than 1cm in diameter6, male gender, and hepatitis B/C virus co-infection7 also increased the risk of developing hypervascularization. The existence of NHHN has significant impact on the prognosis of patients. Previous studies demonstrated higher post-treatment recurrence rates after surgical resection (hazard ratio: 1.94)8 or radiofrequency ablation (hazard ratio: 2.84)6 in patients with NHHNs. In this case, the NHHN transformed into a typical hypervascular HCC after eight months. The patient underwent thermal ablation and achieved a complete response.
In conclusion, EOB-MRI is helpful in detecting the presence of non-hypervascular hypointense hepatocellular nodules on HBP, which tend to show hypervascular and malignant transformation during follow-up. Closely imaging follow-up to identify the HCCs is warranted for appropriate management.
Imaging protocol
Devices used
| MR device used | Signa HDxt 1.5T(GE Healthcare) |
|---|---|
| Autoinjector | LF |
| Workstation | ADW4.5 |
| Contrast enhancement condition | Dose(mL) | Infusion rate (mL/sec) | |
|---|---|---|---|
| Gadoxetate disodium(Gd-EOB-DTPA) | 0.1mL/kg | 1mL/sec | |
| Physiological saline chaser | 30ml | 1mL/sec |
| Imaging type | Imaging sequence | Imaging duration | TE (msec) |
TR (msec) |
FA (deg) |
Fat Sat (Type) |
NEX (Number of additions) |
k-space | Slice thickness (mm) |
FOV (mm) |
Phase direction (Number of steps) |
Lead direction (Number of matrices) |
Slice gap (mm) |
Number of slices |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dual echo | FSPGR (in & out of phase) |
20 sec | 2.2 | 178 | 80 | n | 1 | linear | 8 | 32 | 224 | 256 | 2 | 20 |
| With a contrast agent | ||||||||||||||
| Dynamic | LAVA (axial) |
20 sec | 3.1 (minumum) |
6.7 | 12 | y | 1 | linear | 3 | 32 | 192 | 288 | 0 | 100 |
| DWI | EPI (b=800sec/mm2) |
4 mins 44 sec |
57.1 | 10000 | n | y | 4 | linear | 8 | 32 | 128 | 96 | 2 | 20 |
| T2WI | PROPELLER (axial) |
3 mins | 97 | 6000 | n | y | 1 | linear | 6 | 32 | 256 | 256 | 0 | 34 |
| HBP (20min) |
LAVA (axial) |
20 sec | 3.1 (minimum) |
6.8 | 12 | y | 1 | linear | 3 | 32 | 192 | 288 | 0 | 100 |
References
- InchingoloR, FalettiR, GrazioliL, TricaricoE, GattiM, PecorelliA, et al. MR with Gd-EOB-DTPA in assessment of liver nodules in cirrhotic patients. World J Hepatol. 2018;10(7):462–73.
- TanCH, ChouS, InmuttoN, MaK, ShengR, ShiY, et al. Gadoxetate-Enhanced MRI as a Diagnostic Tool in the Management of Hepatocellular Carcinoma: Report from a 2020 Asia-Pacific Multidisciplinary Expert Meeting. Korean J Radiol. 2022;23(7):697.
- HigakiA, ItoK, TamadaT, TerukiS, YamamotoA, HigashiH, et al. High-risk nodules detected in the hepatobiliary phase of Gd-EOB-DTPA-enhanced mr imaging in cirrhosis or chronic hepatitis: Incidence and predictive factors for hypervascular transformation, preliminary results. J Magn Reson Imaging. 2013;37(6):1377–83.
- SuhCH, KimKW, PyoJ, LeeJ, KimSY, ParkSH. Hypervascular transformation of hypovascular hypointense nodules in the hepatobiliary phase of gadoxetic acid-enhanced MRI: A systematic review and meta-analysis. Am J Roentgenol. 2017;209(4):781–9.
- ChoYK, KimJW, KimMY, ChoHJ. Non-hypervascular hypointense nodules on hepatocyte phase gadoxetic acid-enhanced MR images: Transformation of MR hepatobiliary hypointense nodules into hypervascular hepatocellular carcinomas. Gut Liver. 2018;12(1):79–85.
- LeeDH, LeeJM, LeeJY, KimSH, KimJH, YoonJH, et al. Non-hypervascular hepatobiliary phase hypointense nodules on gadoxetic acid-enhanced MRI: Risk of HCC recurrence after radiofrequency ablation. J Hepatol. 2015 May;62(5):1122-30.
- ChiuN-C, SuC-W, LiuC-A, HuangY-H, ChiouY-Y. Interval to vascularization development in cirrhotic precursor nodules in patients with hepatitis B and C virus co-infections. PLoS One. 2017;12(6).
- ToyodaH, KumadaT, TadaT, NiinomiT, ItoT, SoneY, et al. Non-hypervascular hypointense nodules detected by Gd-EOB-DTPA-enhanced MRI are a risk factor for recurrence of HCC after hepatectomy. J Hepatol [Internet]. 2013;58(6):1174–80. Available from: http://dx.doi.org/10.1016/j.jhep.2013.01.030
- *The case introduced is just one clinical case, so the results are not the same as for all cases.
- *Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


