The usefulness of EOB-MRI in the diagnosis of NAFLD-related HCC
Taipei Veterans General Hospital
Chien-An Liu, Division of abdominal imaging, Department of Radiology, Taipei Veterans General Hospital, Taipei, Taiwan.
Pei-Chang Lee, Division of Gastroenterology and Hepatology, Department of Medicine, Taipei Veterans General Hospital, Taipei, Taiwan.
DATE : 2022
Patient characteristics
Patient’s background
73 years old, Female, 58.4Kg
Disease: Diagnosed NAFLD-related hepatocellular carcinoma
Investigation objectives
This 73-year-old lady has the underlying medical conditions of hypertension, type II diabetes mellitus and severe hepatic steatosis. Besides, she underwent left mastectomy and completed adjuvant chemotherapy for the breast cancer four years ago.
A hypoechoic hepatic mass in segment 6 was accidentally detected on the ultrasonography but the diagnosis could not be made by the triple phase contrast-enhanced CT scan because the lesion was in the context of severe fatty liver. Thereafter, an EOB-MRI was performed to evaluate this hepatic lesion.
Contrast agent used
Gadoxetate disodium(Gd-EOB-DTPA) injection 0.1 mL/kg
Case description
A hepatocellular carcinoma (HCC) other than metastatic cancer was confirmed by the EOB-MRI based on its radiologic characteristics: enhancement on the arterial phase, suspicious washout on the delay phase, hyperintensity on T2-weighted, diffusion restriction and hyperintensity on hepatobiliary phase (HBP). Focal nodular hyperplasia, a common hyperintense tumor at HBP, was excluded from the differential diagnosis due to lack of ring or doughnut-like enhancement.
Curative surgical resection of tumor was arranged for the patient in April 2019. The pathological examination showed a moderately differentiated HCC consisting of acinar / trabecular patterns and bile plugs, which is the so-called green hepatoma, commonly observed in HBP-hyperintese HCC. According to the previous studies, hyperintense HCCs exhibit less malignant behavior and have significantly lower recurrence rates than the hypointense HCCs. Similar to the prior reports, this patient recovered well after surgery and no recurrent tumor has been identified during the follow-up time till now (July, 2022).
Images
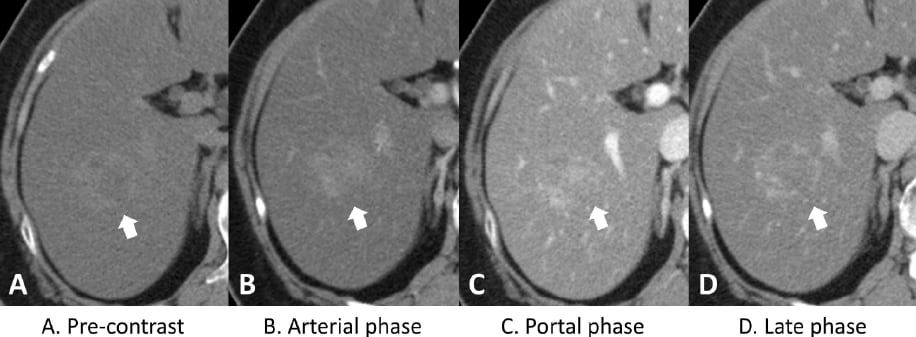
A 3cm ill-defined mass at S6 of liver (arrow) was detected in the background of diffuse hepatic steatosis with decreased attenuation (A). The triple-phase CT scans revealed heterogeneous enhancement of the tumor on the arterial phase (B) and portal phase (C), and without a significant washout on the late phase images(D).
Figure 1. Dynamic computed tomography (CT) of the liver
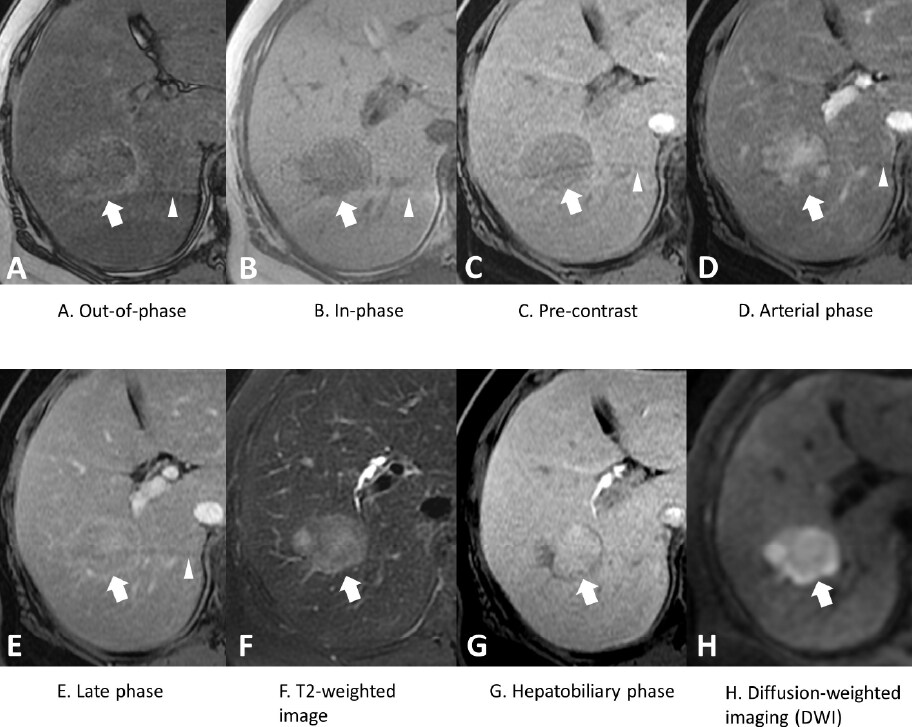
The out-of-phase (A) and in-phase (B) imaging showed significant hepatic steatosis, but no definite fat content was detected in the tumor (arrow). The dynamic contrast-enhanced T1WI images (C, D, E) demonstrated enhancing patterns of tumor similar to those on the CT scans. Besides, enhancement of tumor capsule with washout was identified on late phase (E), rising the suspicion of hepatoma. The tumor showed high signal intensity (SI) on T2WI (F) and restricted diffusion (H). The HBP image obtained in 20 minutes (G) revealed high SI of the tumor, and the diagnosis of green hepatoma was confirmed. Please note that there was a crescent shape ghosting artifact (arrowhead) in the liver, and it was not derived from the administration of Gadoxetate disodium(Gd-EOB-DTPA)
Figure 2. Gd-EOB-DTPA–enhanced magnetic resonance imaging (MRI)
Usefulness of contrast-enhanced MRI with Gadoxetate disodium(Gd-EOB-DTPA) in this case
Nonalcoholic fatty liver disease (NAFLD) has been identified as an important risk factor for HCC1. The most common imaging pattern of fatty liver is diffuse homogeneous fat deposition appearing with low attenuation on CT and signal loss in out-of-phase of chemical shift gradient-echo MRI images2. Diffuse fatty infiltration may obscure an underlying focal hepatic lesion or alter its typical imaging features on CT. MRI is more sensitive for differentiating the target lesion because of its excellent soft-tissue contrast, high spatial resolution, and different imaging sequences3. In this case, this tumor showed heterogeneous contrast enhancement on the arterial phase and became iso-attenuation on late phase images of CT, unlike the typical enhancement pattern of HCC (evident arterial enhancement and washout on portal or equilibrium phase images), and can’t rule out breast cancer with liver metastasis.
Without functioning hepatocytes, most hepatic tumors, including liver metastasis, show hypointensity in the HBP. On the contrary, focal nodular hyperplasia (FNH) and FNH- like lesions reveal hyperintensity in the HBP owing to the uptake of gadoxetic acid (Gadoxetate disodium(Gd-EOB-DTPA)) by hyperplastic normal hepatocytes. In addition to the typical enhancement pattern, HCC commonly reveals low signal intensity in the HBP compared with the liver parenchyma. However, about 10% - 15% of HCCs present hyperintense in the HBP, so-called green hepatoma, and the pathologic and biologic characteristics of preserving the expression of OATP1B3 (an uptake transporter), whereas HBP-hypointense HCCs have lower or no OATP1B3 expression4. More than half of the HBP-hyperintense HCCs are well to moderately (67%) differentiation. Microscopic portal invasion or intrahepatic metastasis is significantly lower in patients with green hepatoma, which contribute to a favorable prognosis than in patients with HBP-hypointense HCC5. In conclusion, EOB-MRI is useful in the diagnosis NAFLD-related HCC and differentiation from metastatic cancer in the context of severe hepatic steatosis.
Imaging protocol
Devices used and contrast conditions
| MRI device | Signa HDxt 1.5T(GE Healthcare) |
|---|---|
| Automatic injection device | LF |
| Work station | ADW4.5 |
| Contrast conditions |
Dose (mL) | Administration rate (mL/s) | Photography timing | |
|---|---|---|---|---|
| Gadoxetate disodium(Gd-EOB-DTPA) | 0.1mL/kg | 1mL/sec | ー | |
| Physiological saline solution for flushing | 30ml | 1mL/sec |
| Imaging type |
Imaging sequence | Imaging duration | TE (msec) |
TR (msec) |
FA (deg) |
Fat Sat (Type) |
NEX (Number of additions) |
|---|---|---|---|---|---|---|---|
| Dual echo | FSPGR (in & out of phase) |
20" | 2.2 | 178 | 80 | n | 1 |
| Contrast agent administration | |||||||
| Dynamic | LAVA(axial) | 20" | 3.1 (minumum) |
6.7 | 12 | y | 1 |
| DWI | EPI (b=800sec/mm2) |
4'44" | 57.1 | 10000 | n | y | 4 |
| T2WI | PROPELLER(axial) | 3' | 97 | 6000 | n | y | 1 |
| HBP(20min) | LAVA(axial) | 20" | 3.1 (minimum) |
6.8 | 12 | y | 1 |
| Imaging type | k-space | Slice thickness (mm) |
FOV (mm) |
Phase direction (Number of steps) |
Lead direction (Number of matrices) |
Slice gap (mm) |
Number of slices |
|---|---|---|---|---|---|---|---|
| Dual echo | linear | 8 | 32 | 224 | 256 | 2 | 20 |
| Contrast agent administration | |||||||
| Dynamic | linear | 3 | 32 | 192 | 288 | 0 | 100 |
| DWI | linear | 8 | 32 | 128 | 96 | 2 | 20 |
| T2WI | linear | 6 | 32 | 256 | 256 | 0 | 34 |
| HBP(20min) | linear | 3 | 32 | 192 | 288 | 0 | 100 |
References
- Orci, L. A. et al. Incidence of Hepatocellular Carcinoma in Patients With Nonalcoholic Fatty Liver Disease: A Systematic Review, Meta-analysis, and Meta-regression. Clin. Gastroenterol. Hepatol. 20, 283-292.e10 (2022).
- Hamer, O. W. et al. Fatty liver: Imaging patterns and pitfalls. Radiographics 26, 1637–1653 (2006).
- Elsayes, K. M. et al. Spectrum of Pitfalls, Pseudolesions, and Misdiagnoses in Noncirrhotic Liver. Am. J. Roentgenol. 211, 97–108 (2018).
- Fujita, N. et al. Hyperintense liver masses at hepatobiliary phase gadoxetic acid– enhanced MRI: Imaging appearances and clinical importance. Radiographics 40, 72–94 (2020).
- Ariizumi, S. I. et al. High-signal-intensity MR image in the hepatobiliary phase predicts long-term survival in patients with hepatocellular carcinoma. Anticancer Res. 39, 4219–4225 (2019).
- *The case introduced is just one clinical case, so the results are not the same as for all cases.
- *Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


