Usefulness of Gadoxetate disodium(Gd-EOB-DTPA) contrast magnetic resonance imaging (EOB-MRI) for diagnosis of recurrent hepatocellular carcinoma (HCC) after radiofrequency ablation (RFA): No.1
Ikeda Municipal Hospital
Drs. Yasuharu Imai, Takumi Igura, Yoshiyuki Sawai, Sachiyo Kogita, and Kazuto Fukuda, Dept. of Gastroenterology
GE Discovery CT750 HD
DATE : 2015
ROLES OF RFA IN HCC TREATMENT
According to scientifically based, Japanese liver cancer treatment guidelines, if the liver damage is at grade A or B, and there is a single tumor, then, irrespective of the tumor diameter, the recommended first-line treatment is hepatectomy, but RFA is an alternative option if the tumor diameter is no more than 3 cm. If there are two or three tumors, and none are more than 3 cm in diameter, either hepatectomy or RFA is recommended. Therefore, RFA is indicated for patients with no more than three tumors that are no more than 3 cm in diameter. At the authors’ hospital, the fundamental treatment algorithm sets RFA as an indicated treatment method.
Hasegawa et al. have collated the results of national follow-up studies performed by the Liver Cancer Study Group of Japan, and found that, in the case of HCC patients with no more than three tumors, all no more than 3cm in diameter, at liver damage grades A or B, the results with hepatectomy were significantly better than with RFA or percutaneous ethanol injection with respect to survival and recurrence rates (J. Hepatol., 2013). On the one hand, 60 to 70% of HCC cases in Japan start with hepatitis C, but hepatitis C patients are aging, and HCC patients are also aging. In connection with the aging of HCC patients, the number of occasions for selecting RFA for treatment is increasing. In addition, development of bipolar RFA systems has enabled no-touch ablation, in which two or more needles are inserted, but the tumor is not punctured directly, and ablation is performed without increasing the intra-tumor pressure, and in addition there has been an increase in the range of indications for RFA approaches, such as RFA of HCC at the liver surface at the same time as generation of artificial ascites, and multi-needle RFA. Furthermore, at the authors’ hospital EOB-MRI is used instead of contrast computed tomography (CT) for thorough examination of nodules detected by ultrasonographic liver cancer screening of chronic liver disease patients, and also for liver cancer screening with ultra-high-risk groups. EOB-MRI has higher diagnostic capability than contrast CT for HCC, including early-stage HCC, and it often detects HCC at early stages, when the tumor diameter is small, and this also is leading to an increase in the number of occasions for RFA performance. On the other hand, when HCC is classified by macroscopic observation, multinodular-fusion-type tumors show high malignancy, and EOB-MRI and contrast ultrasonography have been reported to be useful for preoperative diagnosis of multinodular-fusion-type HCC, so these methods should be used as far as possible if multinodular-fusion-type HCC is suggested by imaging.
USEFULNESS OF EOB-MRI FOR DIAGNOSIS OF POST-RFA RECURRENCE
The annual rate of recurrence after RFA treatment of liver cancer is 15 to 20%, indicating the very high risk of liver cancer development at these sites, so diagnosis of recurrence is very important. There is insufficient evidence to support the intervals in follow-up tests for diagnosis of post-RFA recurrence, or the diagnostic methods used, and in general follow-up involves periodic diagnostic imaging and tumor-marker tests. The tumor-marker tests are generally performed at intervals of 2 to 3 months, and the markers are α-fetoprotein (AFP), AFP-L3, and PIVKA-II. With respect to diagnostic imaging, the present authors have reported the usefulness of EOB-MRI for diagnosis of classical, hypervascular HCC, and early-stage liver cancer (Kogita et al., Eur. Radiol., 2010; Ohnishi et al., Eur. Radiol., 2012), but there have also been numerous reports of EOB-MRI having better diagnostic capability for HCC than contrast CT. At the authors’ hospital, in principle, EOB-MRI is performed at 3-month intervals after RFA. In addition to the high diagnostic capability, various reasons have been put forward for EOB-MRI being appropriate for periodic post-RFA follow-up. One advantage is that, unlike contrast CT, it does not involve radiation exposure. Toyoda et al. have reported that, among postoperative HCC patients, those with whom hypovascular, low-signal nodules were found in the hepatobiliary phase of EOB-MRI showed higher recurrence rates than those without such nodules, that is, they had a higher potential for HCC recurrence, and this difference should be useful for recurrence prediction (J. Hepatol., 2013). In addition, in recent years fusion imaging has often been used to support RFA treatment, but at such times EOB-MRI hepatobiliary phase images are used for reference, and EOB-MRI hepatobiliary phase images have thus been used for reference with numerous patients at the authors’ hospital (Makino et al., Oncology, 2013). In addition, in the authors’ multi-site, prospective, comparative study of EOB-MRI and contrast CT for diagnosis of recurrence after radical RFA of hypervascular HCC, EOB-MRI was found to have higher diagnostic capability for recurrence than contrast CT, and to detect recurrence at an earlier stage.
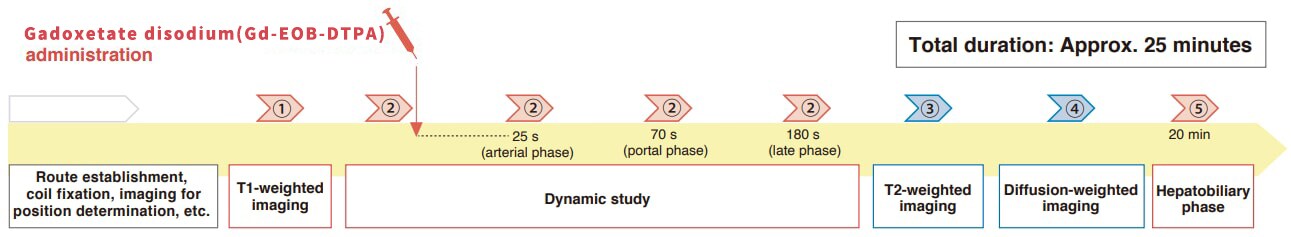
ABDOMINAL MRI METHODS USING GADOXETATE DISODIUM(GD-EOB-DTPA)
Sequence and sequence parameters
| Imaging mechanism and type | Imaging method | Imaging duration | TR (ms) | TE (ms) | FA(º) | NEX | K-space | FOV (mm) | Matrix | Slice thickness (mm) | Gap (mm) | Slice number | Reduction factor | Fat suppression | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ① | T1-weighted imaging | FSPGR (in phase,out ofphase) |
21sec | 175 | 2.1 | 70 | 1 | linear | 360 | 360×192 | 7 | 1.4 | 23 | 2 | - | |
| ② | Dynamic study | LAVA | 18sec | 4.3 | 2.0 | 12 | 1 | linear | 360 | 360×192 | 5 | 2.5 | 84 | 2 | + | |
| ③ | T1-weighted imaging | SSFSE | 17sec | Minimum | 90 | 1 | linear | 360 | 256×224 | 7 | 1.4 | 23 | 2 | ± | ||
| ④ | Diffusion-weighted imaging | EPI (b=1000sec/mm2) |
2min30sec | 6000 | Minimum | 6 | linear | 360 | 128×192 | 7 | 1.4 | 23 | 2 | + | ||
| ⑤ | Hepatobiliary phase | LAVA (axial) |
18sec | 4.3 | 2.0 | 12 | 1 | linear | 360 | 320×192 | 5 | 2.5 | 84 | 2 | + | |
| MRI device used | Signa HDxt 1.5T (GE Healthcare) | |||||||||||||||
Contrast agent and administration method
| Gadoxetate disodium(Gd-EOB-DTPA) | Dose | 0.1mL/kg |
|---|---|---|
| Injection speed | 2mL/sec | |
| Physiological saline solution | Dose | 30mL |
| Injection speed | 2mL/sec | |
| Automatic injection device | Medrad Spectris Solaris EP | |
For reference: Contrast CT standard protocol
| CT device used | Discovery CT 750 HD (GE Healthcare) | |
|---|---|---|
| Iodine contrast agent (300 mg/mL) |
Dose | 2 mL/kg |
| Injection duration | Fixed, 27 s | |
CASE PRESENTATION

Patient’s background and objectives of MRI
Male, 70s.
The patient had type-C cirrhotic.PEG-interferon + ribavirin treatment was ineffective, and HCC developed in S5 of the liver.
EOB-MRI findings

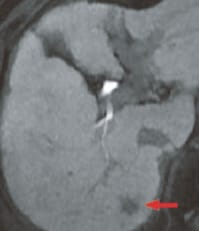
a) Pre-contrast, T1-weighted image

b) Arterial phase

c) Portal phase

d) Late phase
EOB-MRI
e) Hepatobiliary phase
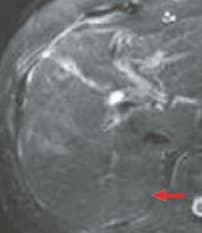
f) Respiratory-synchronized, T2-weighted image
g) In-phase, T1-weighted image
h) Out-of-phase, T1-weighted image
EOB-MRI
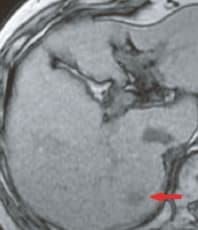
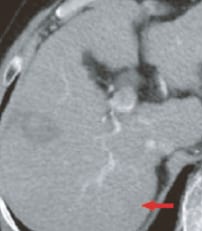
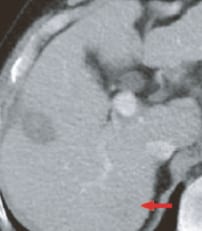
The pre-contrast, T1-weighted image (a) showed a faint low signal, and in the arterial phase (b) rather faint, early-stage dark staining was seen.In the portal phase (c), there was a faint low signal, in the hepatobiliary phase (e) there was a distinct low-signal tumor with a diameter of 15 mm, and this was considered to be typical hypervascular HCC. The respiratory-synchronized, T2-weighted image (f) showed a faint high signal. The in-phase, T1-weighted image (g) showed a faint low signal, and the out-of-phase image (h) showed a decreased signal and the presence of fat.
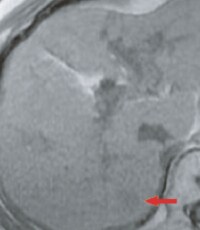
Contrast CT findings
In contrast CT after diagnosis by EOB-MRI (i, j, k), the principal lesion was not detected.
i) Arterial phase
j) Portal phase

k) Equilibrium phasem
Contrast CT
Contrast ultrasonography findings
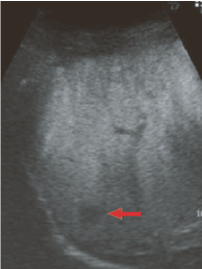
In the arterial phase of contrast ultrasonography, faint, early-stage dark staining was shown (not shown in the figure), and in the Kupffer phase with imaging at high acoustic power (l) defects were shown. A diagnosis of hypervascular HCC was made.
l) Kupffer phase with imaging at high acoustic power
Contrast ultrasonography
Usefulness of EOB-MRI diagnostic imaging results with this patient
In the arterial phase of EOB-MRI, this patient showed a faint high signal (early-stage dark staining), whereas in the hepatobiliary phase a distinct low signal was seen, and diagnosis of HCC was readily achieved with EOB-MRI. On the other hand, no clear tumorous lesions could be detected with CT in the arterial, portal or equilibrium phases. The imaging with B-mode ultrasonography was poor, so, taking the hepatobiliary phase of EOB-MRI as the reference image, RFA was performed under fusion imaging, using a navigation system. In addition, judgment as to therapeutic efficacy was made with fusion of EOB-MRI before and after treatment (Makino et al., Abdom. Imaging, 2015). It can thus be seen that EOB-MRI can be used not only for diagnosis of post-RFA recurrence, but also to support RFA under fusion imaging, and to determine therapeutic efficacy.
Precautions for use
9.Precautions relating to patients with specific background factors (taken from the Package Insert)
9.8 Elderly patients
Administration must be performed with care, and with sufficient monitoring of the patient’s condition. Elderly patients generally have depressed physiological function.
- *The case introduced is just one clinical case, so the results are not the same as for all cases.
- *Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


